Gynecological Cancer
Gynecological cancer refers to any cancer that originates in a female reproductive organ, such as ovarian, cervical, uterine/endometrial, vaginal, and vulvar cancers.1 These cancers have varying symptoms, and as screenings are not available for these cancers except for cervical cancer, it is important for patients and providers to understand and recognize the symptoms for each. This health awareness campaign can help your organization implement evidence-based practices when communicating about gynecological cancer.
Data and Statistics
In 2019, the latest year for which incidence data are available in the U.S., for every 100,000 females, 28 new uterine cancer cases, eight new cervical cancer cases, and ten new ovarian cases were reported.2
Uterine—specifically endometrial—is the most common gynecologic cancer while vaginal is the least common.3 Uterine cancer includes the more common endometrial cancer and the rarer uterine sarcoma.3 Of the gynecological cancers, ovarian cancer is responsible for the most deaths among individuals assigned female at birth in the United States.4
Best Practices for Communicating About Gynecological Cancer
-
Address populations that are at higher risk for gynecological cancer
-
- Honor LGBTQI+ individuals' needs. See “Communicating with Diverse Audiences” below for research-based recommendations and sample messages.
- Highlight health disparities for each cancer type: Cervical cancer incidence is highest among Hispanic and American Indian/Alaska Native (AI/AN) people.2 Black people have the highest incidence of uterine cancer compared to other racial/ethnic groups.2 Hispanic persons are diagnosed with ovarian cancer at a similar rate to White persons2 while White people have the highest incidence of vulvar cancer.5
- Share age-appropriate cancer information. See “Communicating with Diverse Audiences” below for research-based recommendations and sample messages.
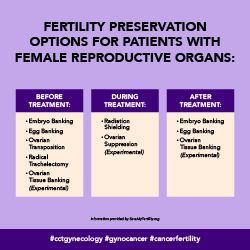
- Consider issues of fertility and family planning that may be affected by gynecologic cancer treatments. To address barriers to fertility and family planning services, such as lack of availability or insurance coverage, refer individuals to resources to alleviate costs and provide psychosocial support.
-
Emphasize gynecologic cancer screening, self-monitoring and follow-up reminders
-
- Remind health care providers that they have an essential role in sharing cervical cancer screening information and encouraging patient screening.6 Patients are much more likely to be screened if a provider recommends it. To ensure patients who have an abnormal cervical cancer screening result receive follow-up care, encourage health systems to establish methods that monitor referrals, follow-up and completion of diagnostic testing.
- There are no screening options for ovarian, uterine, vaginal, endometrial (a type of uterine cancer), and vulvar cancers. Encourage people to pay attention to their bodies and talk to a doctor about any abnormalities, such as unusually timed or heavy vaginal bleeding, bleeding after menopause or other unexplained signs or symptoms that last two weeks or longer.1
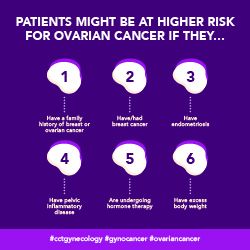
- Remind providers to monitor individuals with increased gynecological cancer risks due to family health history. Having a family history of breast or ovarian cancer can increase a person’s risk for ovarian cancer,7 and a family history of Lynch syndrome is associated with a greater risk of uterine cancer.8
-
Share risk-reducing options
-
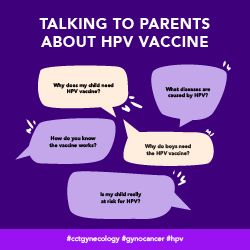
- Furthermore, HPV vaccination substantially reduces the risk of cervical cancer.9 Remind providers to recommend HPV vaccination to the parents of adolescents in a strong, timely, consistent and urgent manner.10 Involve the entire health care team11 to encourage vaccination and the scheduling of follow-up appointments.
- Help people understand their individual risk factors. For example, having a genetic mutation or syndrome may increase risk of ovarian cancer and uterine cancer for some people.12 Encourage genetic counseling and testing when appropriate.
- Share a range of resources specific to cervical, ovarian, uterine, vaginal and vulvar cancers.
- Encourage individuals to stop smoking, as it increases the risk of vaginal cancer and cervical cancer.13
- Inform decision-makers about the effectiveness of built environment improvements, such as sidewalks and standalone bike lanes, to increase physical activity. Obesity is strongly linked to uterine cancer14 and other gynecologic cancers.15
-
Encourage health system improvements to survivorship care and resources
-
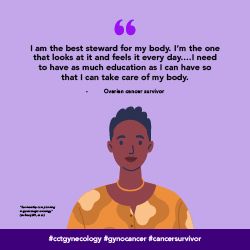
- Remind providers to share information that can help survivors monitor and understand long-term treatment symptoms and side effects. Doing so can help survivors make informed decisions on when to seek additional screenings.16
- Some cancer survivors may value spiritual and psychological wellness;16 therefore, encourage providers to refer patients to behavioral health specialists.
- Providers have expressed the need for resources they can share with patients to help them return to normal life without fear or anxiety.16 Share information that can better equip providers to have these conversations.
- Some gynecologic oncologists cite time concerns as a main barrier to conducting survivorship discussions and providing patients with survivorship care plans (SCP).16 Encourage providers to engage with dedicated survivorship care specialists who can tailor disease-specific SCPs and support provider-patient discussions on survivorship care.
-
Refer Gynecological Cancer patients to clinical trials
-
- Individuals with Limited English Proficiency (LEP), particularly Black and Hispanic persons with LEP, are underrepresented in gynecologic clinical trials.17 Work with translators and linguistically diverse providers to communicate across different health literacy levels.
- Encourage providers to inform Black individuals of phase one clinical trials studying gynecologic cancers, an area in which they are statistically underrepresented.18
Communicating with Diverse Audiences
Communication-related issues may also play a role in cancer disparities.19 Consider the information most useful to each diverse group (see below for specific messaging and read more on health disparities here). Tailor communication to these populations of focus with messages that also address conditions where these communities live, learn, work and play, as these social determinants of health can impact a wide range of health risks and outcomes. To ensure messages resonate with the coalition’s intended audience, we also recommend referring to the National Networks’ existing resources and adapting messages to reflect individuals with lived experiences.
-
Black/African American
-
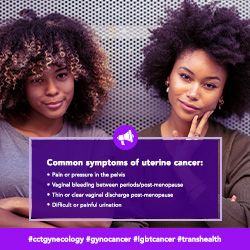
- Black persons experience the highest incidence rates of uterine cancer, with 29 uterine cancer cases per 100,000, compared to 28 cases per 100,000 among non-Hispanic White women.2 Black persons also experience the highest mortality rates, with nine non-Hispanic Black persons per 100,000 dying from uterine cancer compared to five per 100,000 among non-Hispanic White persons. Share these statistics and information about uterine cancer symptoms alongside imagery of Black individuals.
-
Hispanic/Latinx/o/a
-
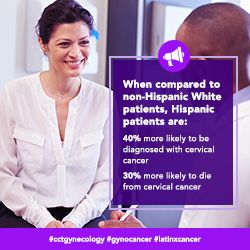
- Hispanic persons are 40 percent more likely to be diagnosed with cervical cancer and are 30 percent more likely to die from cervical cancer, as compared to non-Hispanic White persons.20 Share these statistics and information about cervical cancer screenings alongside imagery of Hispanic individuals.
-
AANHPI (Asian American, Native Hawaiian/Pacific Islander)
-
- AANHPI individuals tend to have a lower incidence of uterine, vulvar and cervical cancers compared to White persons.2 However, it is still important to share information about these cancer types and associated symptoms to encourage appropriate screening and/or follow up care. Share this information alongside imagery of AANHPI individuals.
-
AI/AN (American Indian/Alaska Native)
-
- When compared to non-Hispanic White persons, AI/AN individuals experienced higher incidences of cervical cancer, as well as higher mortality rates.21 Encourage routine screenings for cervical cancer and follow up of abnormal test results alongside imagery specific to a particular Tribal community.
- For some AI/AN patients, spiritual care may be just as important as physical and mental components of care.22 Factors such as separation from family and tribal communities can leave individuals feeling spiritually vulnerable and may deter patients from seeking or continuing care. Craft messages informed by the lived experiences of AI/AN cancer survivors, spiritual leaders, and community and ceremonial elders to demonstrate cultural competency in care practices.
-
LGBTQI+
-
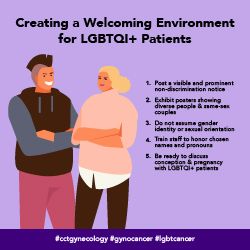
- LGBTQI+ patients and survivors report fears of social stigmas as well as experiencing stigma within health care settings.23 Create messages that help health providers to recognize and overcome implicit bias when communicating with individuals with gynecological cancer. This may help to reduce stigma and to foster trust and honesty.
- Honor LGBTQI+ patients’ needs. Most transgender men and some gender nonconforming individuals require cervical cancer screening. Lesbian individuals should continue to be screened for cervical cancer.24 Share guidelines from the National LGBT Cancer Network for tips on making care more comfortable for LGBTQI+ individuals.25 Messages can also refer providers to the National LGBT Cancer Network’s self-guided training modules on cultural competency
- Transgender men report avoiding medical care in situations that require them to educate providers on transgender health.26 Educate providers on gender-affirming language, as well as the use of hormones and surgical interventions when caring for transgender persons.
-
SES (socioeconomic status)
-
- Share messaging that encourages smoking cessation, as studies show many cervical cancer survivors of lower SES did not associate smoking habits with increased cancer risk.27 Share resources for non-judgmental social support and methods for coping with tobacco cravings.
-
Age-based messaging
-
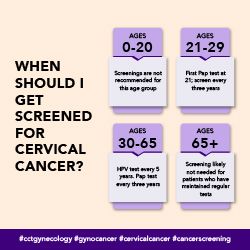
- Share age-appropriate cancer information: Cervical cancer screening should start at age 21 and HPV vaccination can start at age 9,28 while uterine cancer usually presents after age 50. Vaginal and vulvar cancers are generally diagnosed at older ages (median age of 67).3
-
Rural
-
- Research shows that individuals living in rural areas are 63% less likely to be referred to a gynecologic oncologist for surgery as compared to individuals in urban areas.29 However, in instances where they are referred, rural individuals are just as likely to receive surgery. Share messages that encourage providers to not only provide referrals to a surgical specialist, but also connect with local community resources to help rural individuals overcome any potential treatment barriers.
Gynecological Cancer Messages and Graphics
Download All Messages and Graphics How to Post on Social Media
|
Topics |
Suggested Images |
|---|---|
|
Topic: Helping patients understand risk factors for ovarian cancer #cctgynecology #gynocancer #ovariancancer #cdc #dcpc |
|
|
Topic: Promoting healthy behaviors for survivors #cctgynecology #gynocancer #cancersurvivor #cdc #dcpc |

|
|
Topic: Giving survivors the tools to monitor their own health #cctgynecology #gynocancer #cancersurvivor #cdc #dcpc |
|
|
Topic: Give providers resources to find appropriate gynecologic cancer clinical trials #cctgynecology #gynocancer #cancertrials #cdc #dcpc |

|
|
Topic: Sharing resources for non-English speaking patients #cctgynecology #gynocancer #cdc #dcpc |

|
|
Topic: Tips for caring for LGBTQI+ patients #cctgynecology #gynocancer #lgbtcancer #cdc #dcpc |
|
|
Topic: Tips for caring for transgender patients #cctgynecology #gynocancer #lgbtcancer #transhealth #cdc #dcpc |

|
|
Topic: Considering the effects of hormone therapies when caring for transgender patients #cctgynecology #gynocancer #lgbtcancer #transhealth #cdc #dcpc |

|
|
Topic: Encourage cervical cancer screenings for American Indian and Alaska Native patients #cctgynecology #gynocancer #cervicalcancer #aian #cdc #dcpc |

|
|
Topic: Uterine cancer awareness for Black patients #cctgynecology #gynocancer #uterinecancer #blackhealth #cdc #dcpc |
|
|
Topic: Cervical cancer awareness for Hispanic patients #cctgynecology #gynocancer #latinxcancer #cdc #dcpc |
|
|
Topic: Encourage age-based cervical cancer screenings #cctgynecology #gynocancer #cervicalcancer #cancerscreening #cdc #dcpc |
|
|
Topic: Encourage HPV vaccinations for adolescents and young adults #cctgynecology #gynocancer #hpv #cdc #dcpc |
|
|
Topic: Share family-planning and fertility resources #cctgynecology #gynocancer #cancerfertility #cdc #dcpc |
|
|
Topic: Vulvar cancer awareness for ages 60+ #cctgynecology #gynocancer #vulvarcancer #cdc #dcpc |

|
|
Topic: Behavioral health resources for gynecologic cancer survivors #cctgynecology #gynocancer #cdc #dcpc |

|
|
Topic: Encouraging smoking cessation + providing cessation resources/strategies for low-SES patients #cctgynecology #gynocancer #quitsmoking #cdc #dcpc |

|
Download All Messages and Graphics How to Post on Social Media
How to Post to Social Media
Start by downloading the ZIP file above. Then double click the downloaded file to unzip and open the folder. Inside, you’ll find three CSV files.
- Messaging.csv contains captions for all messages in the toolkit, organized by topic.
- Bulk - Instagram.csv contains captions for all Instagram messages, along with graphics URLs that can be used to bulk schedule both text and images.
- Bulk - LinkedIn-Facebook-Twitter.csv contains captions for all LinkedIn, Facebook, and Twitter messages, along with graphics URLs that can be used to bulk schedule both text and images.
Inside the main folder, you’ll also see two sub-folders containing the messaging graphics for all major platforms. The first folder contains rectangular images suited for use on Facebook, Twitter, and LinkedIn. The second folder contains square images suited for Instagram.
Select your platform below for additional instructions.
-
Facebook
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Facebook. If you aren’t already logged in, enter your email address (or phone number) and password, then tap “Log in.”
- Tap the post box. This box is at the top of the News Feed. If you're posting to a group, you’ll find the box just below the cover photo. There will generally be a phrase like “Write something”or “What’s on your mind?” in the box.
- Tap “Photo/Video” near the middle of the post screen, then select the downloaded graphic to upload and tap “Done.” Doing so adds the photo to your post.
- Tap “Post.” It’s in the top-right corner of the screen from the app, or the bottom-right from your computer. Doing so will create your post and add it to the page you’re on.
-
Twitter
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Twitter. If you aren’t already logged in, enter your email address and password, then tap “Log in.”
- Tap the post button. This button is at the bottom right of the News Feed. There will generally be a phrase like “What’s happening?” in the box.
- Tap the camera icon near the middle of the post screen, or the picture icon in the bottom left of the post screen then select the downloaded graphic to upload, and add the post caption.
- Tap “Tweet.” It’s in the top-right corner of the screen from the app, or the bottom-right from your computer. Doing so will create your post and add it to the page you’re on.
-
Instagram
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Instagram. If you aren’t already logged in, enter your username (or phone number) and password, then tap “Log in.”
- Tap the plus sign box. This box is at the top right. Select the downloaded graphic or drag it into the box to upload it.
- Select “Square (1:1)” for the aspect ratio, then click “Next.”
- Ignore the filters screen, then click “Next” again.
- Paste the caption where it says, “Write a caption…” at the top.
- Under “Accessibility,” consider adding alt text to describe the photo for people with visual impairments.
- Tap “Share.” It's in the bottom-right corner of the screen.
-
LinkedIn
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open LinkedIn. If you aren’t already logged in, enter your email address and password, then tap “Log in.”
- Tap “Start a post” from the main share box. This box is at the top of your profile.
- Tap “Photo” from the top of the post screen, then select the downloaded graphic to upload and tap “Done.” Doing so adds the photo to your post.
- Tap “Post.” It's in the the bottom-right. Doing so will create your post and add it to the page you’re on.
-
Bulk Scheduling
-
Social media management tools like Hootsuite and Sprout Social offer bulk scheduling options for uploading multiple messages at once. The spreadsheets included in the download can be adapted to fit multiple scheduling platforms or services. They are currently formatted to work with Sprout Social’s bulk scheduling option. Please review the bulk scheduling format requirements for your specific platform before posting. Messages are sorted by network.
Gynecological Cancer Resources
|
Resource |
Description |
|---|---|
| Foundation for Women’s Cancer |
Providing education and increasing awareness about gynecologic cancer risk, prevention, early detection and treatment. |
| CancerCare Gynecological Cancers Patient Support Group |
A free, 15-week support group for patients living with gynecological cancer who are currently in treatment. |
| Latinas Contras Cancer |
An organization providing cancer education, patient navigation, and survivorship services for Latinos in Spanish and English. |
| SaveMyFertility |
A resource for adult cancer patients and the parents of children with cancer who want to learn more about preserving their fertility before and during cancer treatment, as well as protecting their hormonal health after treatment. |
| Alliance for Fertility Preservation |
Increasing access to information and resources regarding fertility preservation for cancer patients and healthcare professionals. |
| Resolve |
Providing financial resources for family building. May be helpful for patients facing infertility and/or those who have the option of fertility preservation before cancer treatment. |
| FORCE |
Improve the lives of individuals and families facing hereditary cancer through education, advocacy, and research. |
| National Ovarian Cancer Coalition |
Supporting survivors of ovarian cancer and their caregivers, and funding research to advance treatment and find a cure. |
| The National Cervical Cancer Coalition |
Helping women, family members and caregivers battle the personal issues related to cervical cancer and HPV and advocating for cervical health in all women. |
| Cervical Cancer Awareness Month Campaign |
This cervical cancer awareness month campaign can help your organization implement evidence-based practices when communicating about cervical cancer. |
| Gay and Lesbian Medical Association |
A group dedicated to ensuring health equity for LGBTQ+ people through research, advocacy, and education. GLMA also shares resources for both patients and providers caring for LGBTQ+ people. |
| Prevention and Early Diagnosis of Ovarian Cancer and/or Uterine Cancer (e-modules) |
A group dedicated to ensuring health equity for LGBTQ+ people through research, advocacy, and education. GLMA also shares resources for both patients and providers caring for LGBTQ+ people. |
References