About Lung Cancer Awareness Month
Lung Cancer Awareness Month is an annual observance held throughout the Month of November. It is intended to raise awareness of lung cancer and to promote research into its cause, prevention, diagnosis, treatment, survivorship and cure. According to the Centers for Disease Control and Prevention (CDC), “more people in the United States die from lung cancer than any other type of cancer” (2020).
Data and Statistics
In 2018, the latest year for which incidence data are available, in the United States, 218,520 new cases of lung and bronchus cancer were reported, and 142,080 people died of this cancer. For every 100,000 people, 54 new lung and bronchus cancer cases were reported and 35 people died of this cancer (U.S. Cancer Statistics Working Group, 2021).
Best Practices for Communicating About Lung Cancer
Promote patient-provider discussions of lung cancer risk
- Lung cancer risk factors include smoking, secondhand smoke exposure, radon and other environmental exposures such as asbestos, and personal or family history (CDC, n.d.). Encourage patient-provider discussions of ways to reduce these risks.
- Familial history of lung or other cancers may increase risk for lung cancer in nonsmokers (Kanwal, Ding and Cao, 2017). Encourage patient-provider discussions of family history and risk.
- Having a family history is associated with a higher perceived risk of lung cancer among current or former smokers. This can influence a person’s willingness to pursue lung cancer screening (Turner et al., 2021). Provide information about the link between family history and lung cancer risk.
- Radon exposure can increase a person's risk of lung cancer, especially in nonsmokers. It is estimated that about 20,000-40,000 nonsmokers get lung cancer each year, with 2,900 cases estimated to be associated with radon (CDC, n.d.). Encourage patient-provider discussions of screening for lung cancer among these individuals.
Provide information about lung cancer screening and promote screening among the individuals that are recommended to be screened
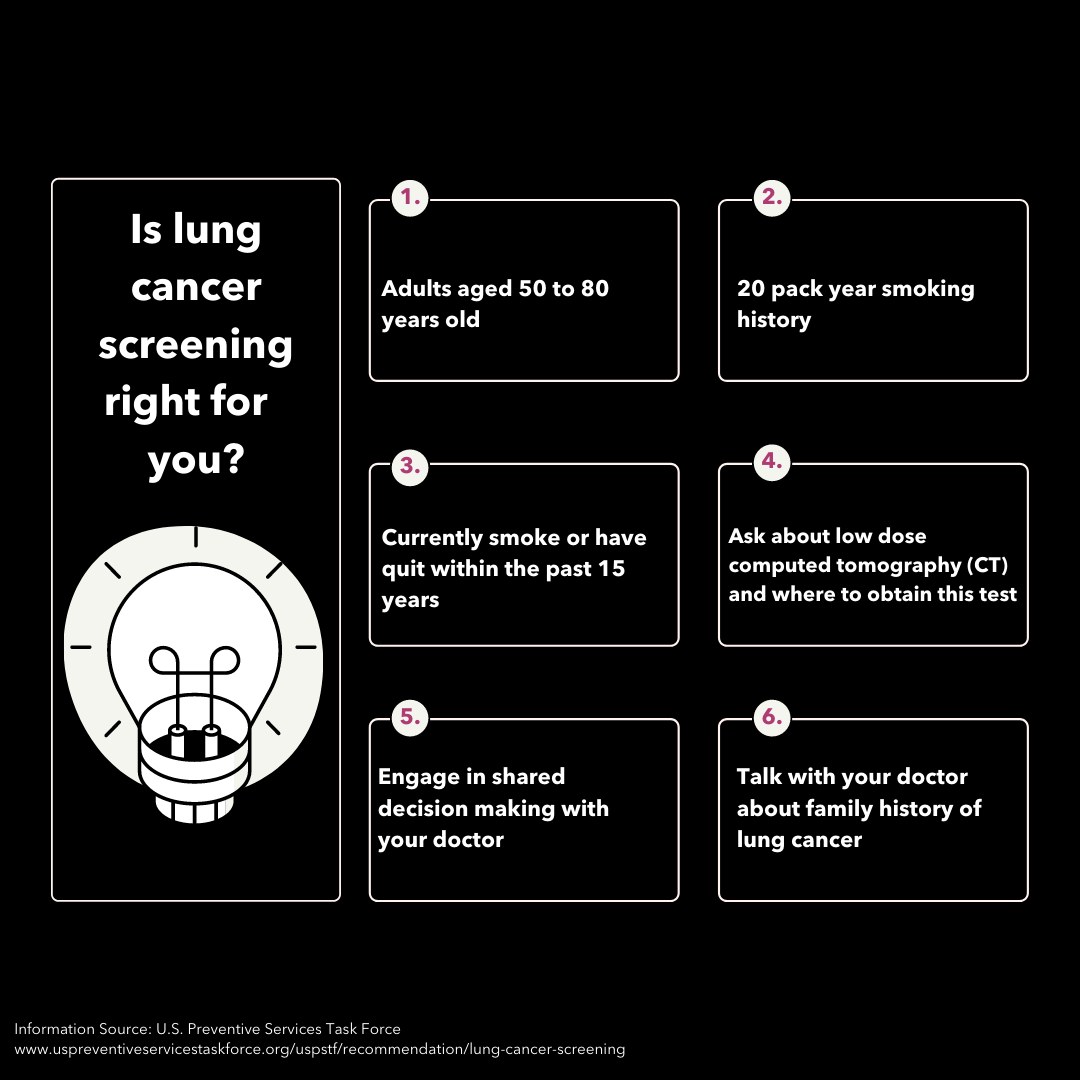
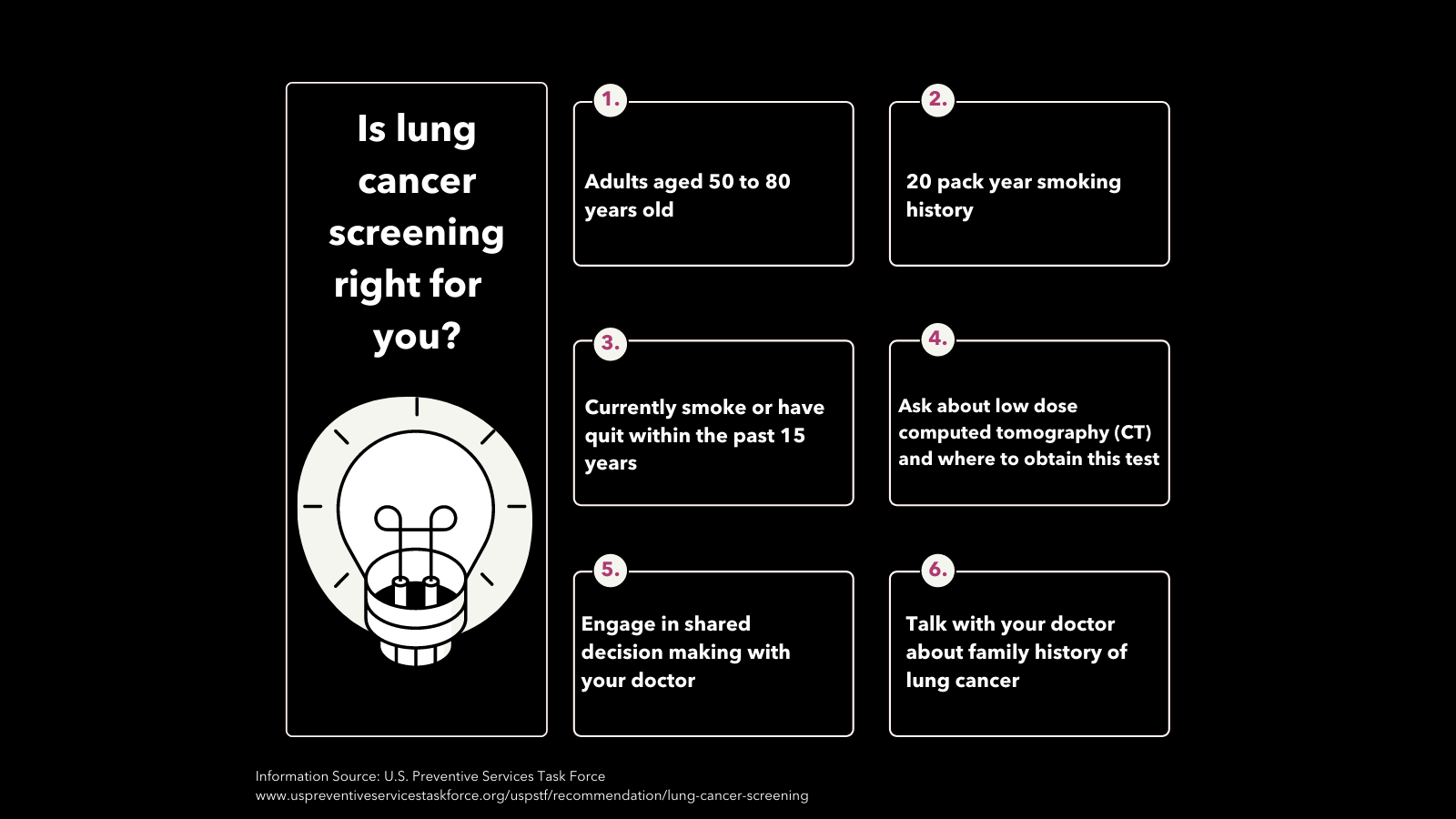
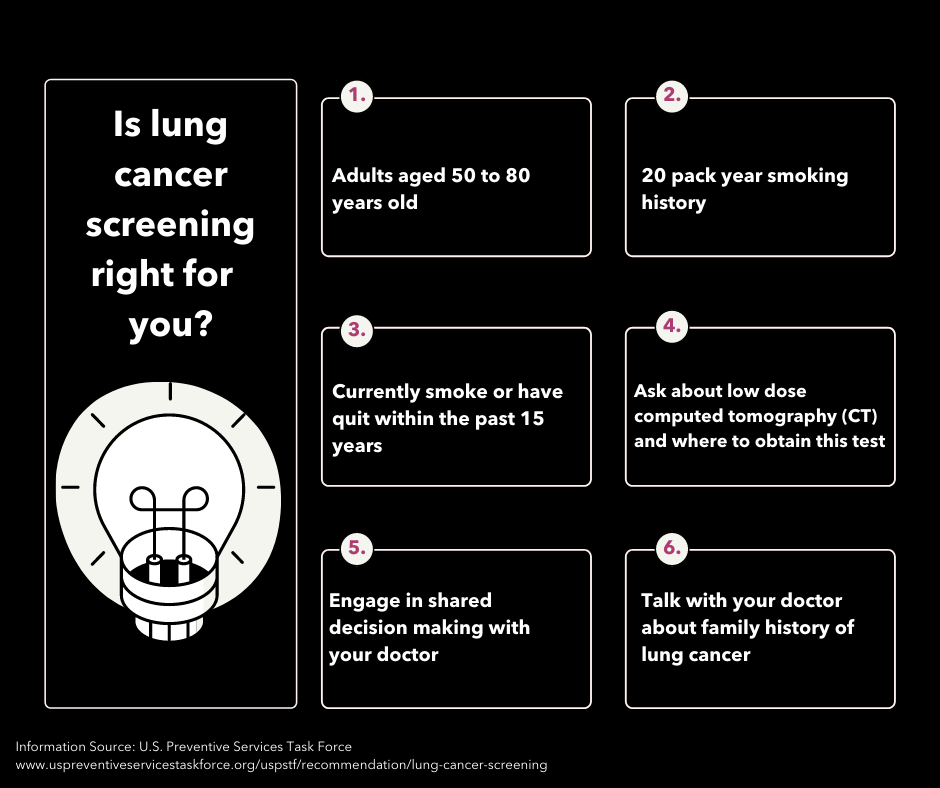
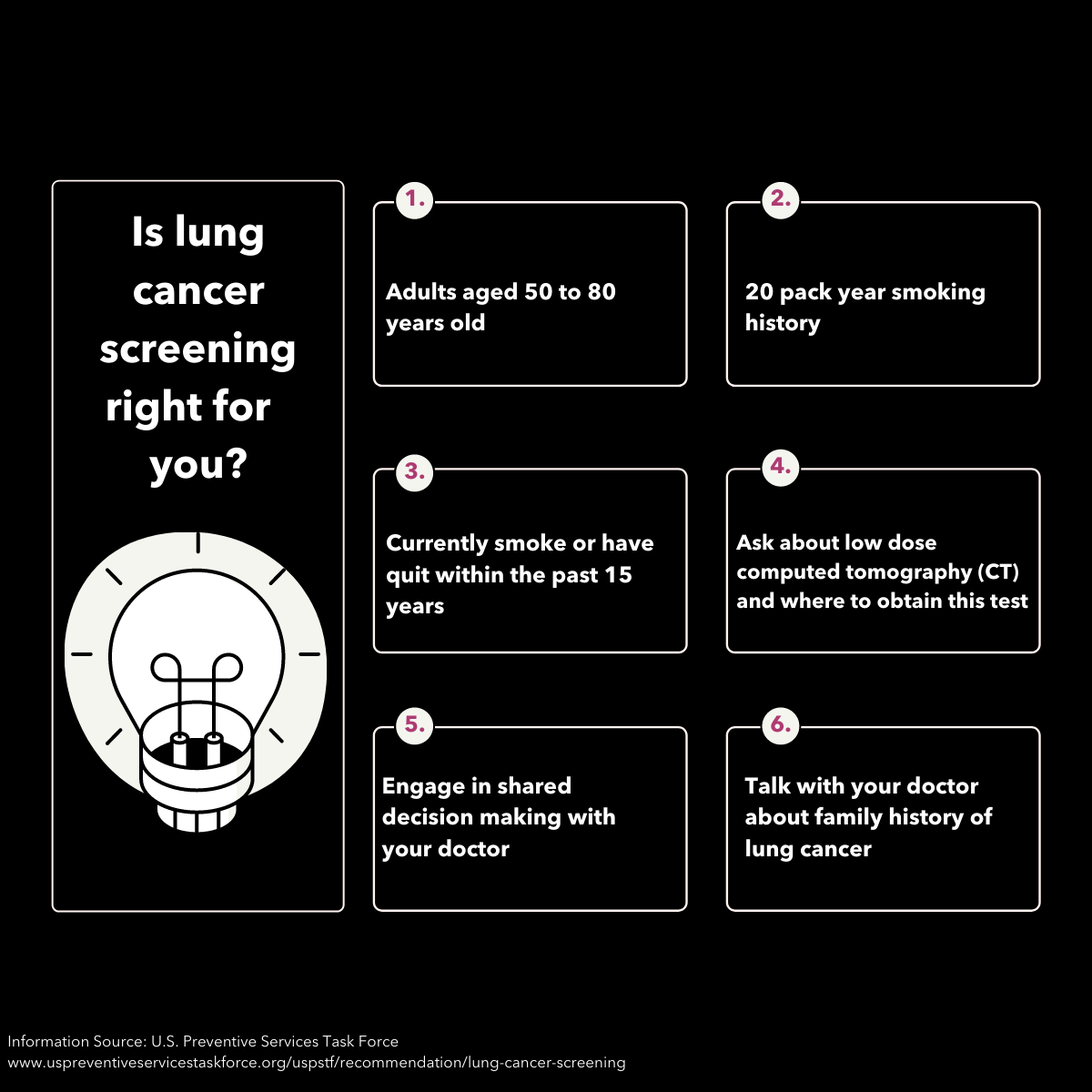
- The U.S. Preventive Services Task Force (USPSTF) recommends yearly lung cancer screening with low-dose computed tomography (also called a low-dose CT scan, or LDCT) for people who have a 20 pack-year or more smoking history, and smoke now or have quit within the past 15 years, and are between 50 and 80 years old (CDC, n.d.). Encourage patient-provider discussions of screening for lung cancer among these individuals.
Provide information about long-term care and survivorship issues in addition to treatment information
- Follow-up care to lung cancer survivors should focus on tobacco cessation, increased physical activity, maintaining appropriate body weight, and limiting alcohol consumption, in addition to ongoing vaccinations, regular cancer screenings and pain management (Arem et al., 2020 & Underwood et al., 2012). When creating messaging for lung cancer survivors focus on these topics.
- The American College of Surgeons recommends and encourages Commission on Cancer (CoC)-accredited programs to provide a survivorship care plan to patients completing cancer treatments (American College of Surgeons, 2020). Encourage providers to promote survivorship care plans for patients.
- Inform patients and caregivers about available resources they can request, such as survivorship care plans or long-term recommendations about screening and follow-up.
- The introduction of palliative care early in the course of treatment may prolong survival and improve quality of life for patients with advanced lung cancer (Sullivan et al., 2019). Promote patient-provider discussion of palliative care options.
Remind providers about the importance of communication and its impact on patients’ quality of life
- Cancer patients, survivors and caregivers often face “cancer information overload” and may feel overwhelmed by information, which can lead to avoidance of cancer information when having to make an important health decision (Chae, 2016). Reduce cancer information overload in your communication strategy.
- Patients frequently report health professionals, such as doctors and nurses, as their most important information source (Mekuria, Erku & Belachew, 2016). Emphasize the important role that providers have in addressing the information needs of patients and caregivers.
- Research suggests that Black persons continue to face barriers to accessing high quality, patient-centered care, specifically relating to specialty care, medical tests, and patient-provider communication (Mitchell et al., 2020). Create messages recognizing the influence of implicit bias.
- People who smoke and groups with a lower socioeconomic status often perceive barriers to lung cancer screening. Barriers include feeling blamed for ill health, stigma, and misbelieving that lung cancer is not treatable (Quaife et al., 2016). When screening is recommended, messages should be tailored, nuanced and address these barriers.
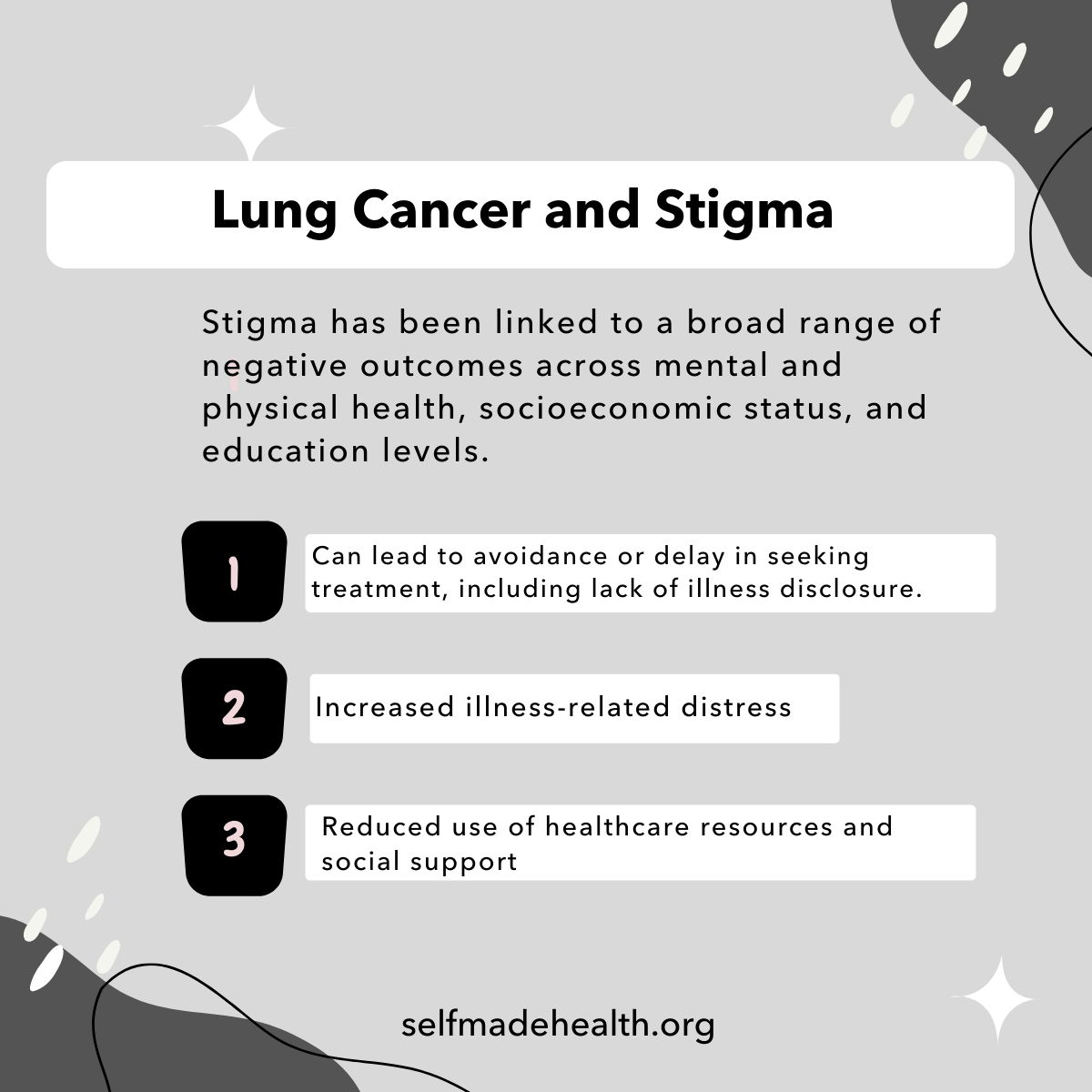
Address and combat stigma often associated with a lung cancer diagnosis
- Lung cancer is often socially stigmatized, which can lead to emotional distress, increased physical symptoms and decreased quality of life (Williamson et al., 2021). Providers should avoid stigmatizing the illness and be aware of the influence of societal stigma on both smokers and nonsmokers with lung cancer.
- Stigmatization can deter patients from seeking medical support for symptoms, limit their involvement in lung cancer treatment and survivorship care (Hamann et al., 2018). Address lung cancer stigma in your messaging to promote medical help–seeking behavior.
Communicating with Diverse Audiences
Certain groups experience disparities in lung cancer screening, incidence, mortality, and survival (National Cancer Institute, 2020). Cancer health disparities are complex and affected by various factors, such as, social determinants of health, behavior, biology, genetics, and more (National Cancer Institute, 2020). Communication-related issues may also play a role in cancer disparities (White-Means and Osmani, 2017). Consider the information most useful to each diverse group. CDC's Chronic Disease Center provides a framework for achieving health equity by addressing the social determinants of health, including examples of community programs (CDC, n.d.)
Below you will find considerations for specific audiences, including: Black/African American, Hispanic/Latinx, Asian Americans, Native Hawaiians and Pacific Islanders [AANHPI], and American Indian/Alaskan Native [AI/AN].
Lung cancer is the second most commonly diagnosed cancer in both Black men and women. According to 2019 estimates, about 36,840 Black men and 36,190 Black women were expected to die from lung cancer, making it the leading cause of cancer-related death among Black persons. (American Cancer Society, 2019). Additionally, Black persons with lung cancer were 16% less likely to be diagnosed early compared to White persons (American Lung Association, 2020). According to the Center for Black Health & Equity, health disparities for Black persons “can be linked to delayed diagnosis, lack of health insurance and inadequate access to quality cancer treatment and poor patient care” (Center for Black Health & Equity, n.d.). CDC has specific resources for communication with African American men at African-American Men and Lung Cancer Infographics.
Lung cancer is the most common cause of cancer death for Latinx men and the second most common cause of cancer death for Latinx women (Miller et al., 2021). Latinx persons with lung cancer were 39% more likely to not receive treatment for their cancer compared with White persons (American Lung Association, 2020). Furthermore, since cancer incidence among Latinx persons varies by nativity, Hispanic origin group, and duration of U.S. residence, understanding language barriers and cultural differences may help with cancer control efforts (Miller et al., 2021).
Lung cancer is the most common cancer for both AANHPI men and women, with Filipino and Vietnamese persons having the highest rates of lung cancer related deaths (Asian Pacific Partners, 2019). Asian American persons with lung cancer were 15% less likely to be diagnosed early compared to White persons (American Lung Association, 2020). Additionally, the diversity within the AANHIP population in terms of socioeconomic status, immigration patterns, and English proficiency is reflected in differences in risk factors and use of cancer screenings (Torre et al., 2016). Cancer control strategies that focus on cultural and linguistic appropriate approaches, doctors’ recommendations, and improving access to healthcare and patient navigation have shown success for these communities (Torre, et al., 2016).
Lung cancer is the leading cause of cancer death among AI/AN populations due to high commercial tobacco use rates (Centers for Disease Control, 2019). Lung cancer incidence and mortality rates are highest in the Northern Plains and Alaska and lowest in the Southwest (National Native Network, n.d.). Tobacco has historically been and presently remains a sacred and traditional medicine for many Tribal communities (Boudreau, 2016). However, commercial tobacco is sometimes erroneously used in place of traditional tobacco for ceremonies, which exposes Tribal communities to secondhand smoke and increases the risk of lung cancer (National Native Network, n.d.). Lung cancer interventions and commercial tobacco cessation outreach for AI/AN populations should be tailored to the Tribe’s unique culture and barriers (Underwood, 2014).
Lung Cancer Resources |
|
|---|---|
| Resource |
Description |
| American Lung Association: Help and Support Resources | A strong support system can positively impact health outcomes. Connect with these resources offered by the American Lung Association, including specific support related to COVID-19. |
| American College of Radiology | Use the search form to find imagining facilities in your area that are accredited by the American College of Radiology, especially ACR Designated Lung Cancer Screening Centers. |
| Are You At Risk for Radon? | The CDC released this YouTube video to explain the risks of radon exposure and what people can do to mitigate it. |
| ASPIRE Network | The Asian American, Native Hawaiian, and Pacific Islander Network to Reach Equity in Tobacco Control and Cancer (ASPIRE) Network aims to build community capacity and facilitate the development of tobacco and cancer policy initiatives among diverse Asian American, Native Hawaiian, and Pacific Islander (AANHPI) communities across the United States. It is funded through the Centers for Disease Control and Prevention’s Office on Smoking and Health and the Division of Cancer. |
| CDC Statistics and Information on American Indian and Alaska Native Populations | Lung cancer is the leading cause of cancer death among American Indian/ Alaska native men and women. Learn more from the CDC about this incidence and possible risk factors. |
| Comprehensive Cancer Control Webinar Series on Lung Cancer | The American Cancer Society CCC conducted a series of webinars on lung cancer control in 2020. Topics ranged from tobacco cessation to lung cancer screening. |
| Lung Cancer Atlas | The Lung Cancer Atlas is presented by the National Lung Cancer Roundtable and the American Cancer Society. This atlas offers an interactive geographic view of data pertaining to lung cancer in the USA. |
| Lung Cancer: A Guide for Patients & Caregivers | Created by Johns Hopkins University, this guide will help patients understand their diagnosis and provide information for patients, family, and loved ones. |
| National Lung Cancer Roundtable (NLCRT) | The NLCRT is a national coalition of public, private, and voluntary organizations, and invited individuals, dedicated to reducing the incidence of and mortality from lung cancer in the United States through coordinated leadership, strategic planning, and advocacy. |
| National Lung Cancer Roundtable Lung Cancer Screening Webinar Series | The U.S. Preventive Services Task Force, the American Cancer Society National Lung Cancer Roundtable, in partnership with the ACR®, American Academy of Family Physicians, American Thoracic Society, and American College of Chest Physicians, will host a monthly webinar series from June 30–November 17, featuring perspectives from key stakeholder groups, including patients, primary care physicians, pulmonologists, radiologists, epidemiologists, behavioral scientists, oncologists and thoracic surgeons. |
| National Native Network: Keep It Sacred | A national network of Tribes, tribal organizations and health programs working to decrease commercial tobacco use and cancer health disparities among American Indians and Alaska Natives (AI/AN) across the U.S. The resource offers technical assistance, culturally relevant resources, and a place to share up-to-date information and lessons learned, as part of a community of tribal and tribal-serving public health programs. |
|
Nuestras Voces: Prevencion y control del tabaquismo (Spanish Translation: Prevention and Tobacco Control) |
Nuestras Voces Network partnered with the New Mexico Tobacco Use Prevention and Control Program, and the New Mexico Association of Community Health Workers/Nuestra Salud to develop these resources to help community health workers address commercial tobacco control among Hispanics. Two additional supporting tools were also developed in Spanish to address nicotine dependence and family intervention support. These resources are available at: https://bit.ly/MaterialesCHW |
| Product, Substance-Use, and Demographic Characteristics of Hospitalized Patients in a Nationwide Outbreak of E-cigarette, or Vaping, Product Use-Associated Lung Injury (CDC) | While the CDC continues to research the effects of e-cigarettes and vapes, they recommend that the best way to ensure no risk of negative outcomes is to refrain from the use of these types of products. Use this source to learn more. |
| Tobacco Cessation for Cancer Survivors: A Resource Guide for Local Health Departments | Here is a guide from NACCHO on the role of local health departments in minimizing the impact of cancer in their communities. |
| Tobacco Cessation Tools and Resources | Learn how to incorporate the “5 As”- Ask, Advise, Assess, Assist, and Arrange into a patient’s tobacco quit attempt. Here is some information from ASCO on tobacco cessation treatment. |
Lung Cancer Awareness Month Messages and Graphics
| Message | Suggested Graphic |
|
Each year, 140,000+ Americans die from #LungCancer. That's about 383 deaths every day. But you can reduce your risk. Find out more: http://bit.ly/2OS74wV |
|
|
Tobacco use is the leading cause of preventable disease and death in the United States. Get the facts: http://bit.ly/2xW3trc |
|
|
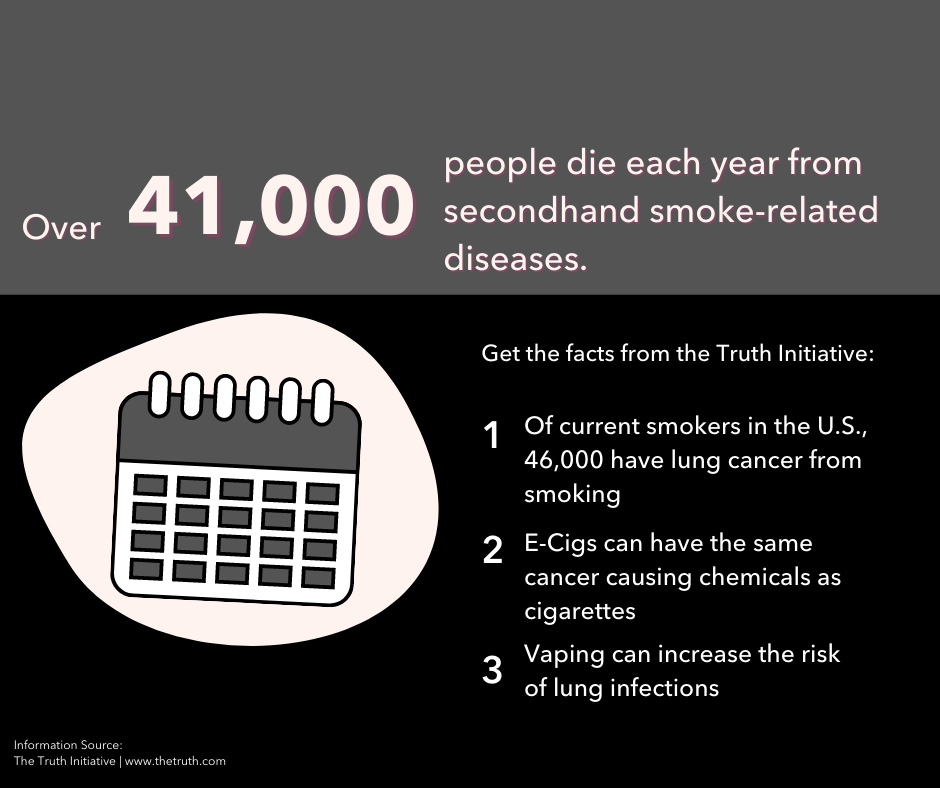
Get the facts about health risks associated with smoking from @TruthInitative http://bit.ly/2asftHJ #FinishIT |

|
|
Get your home tested for radon! Radon is the 2nd leading cause of #lungcancer. Radon is a radioactive gas found in nearly all soils: http://bit.ly/2wxvd2u |

|
|
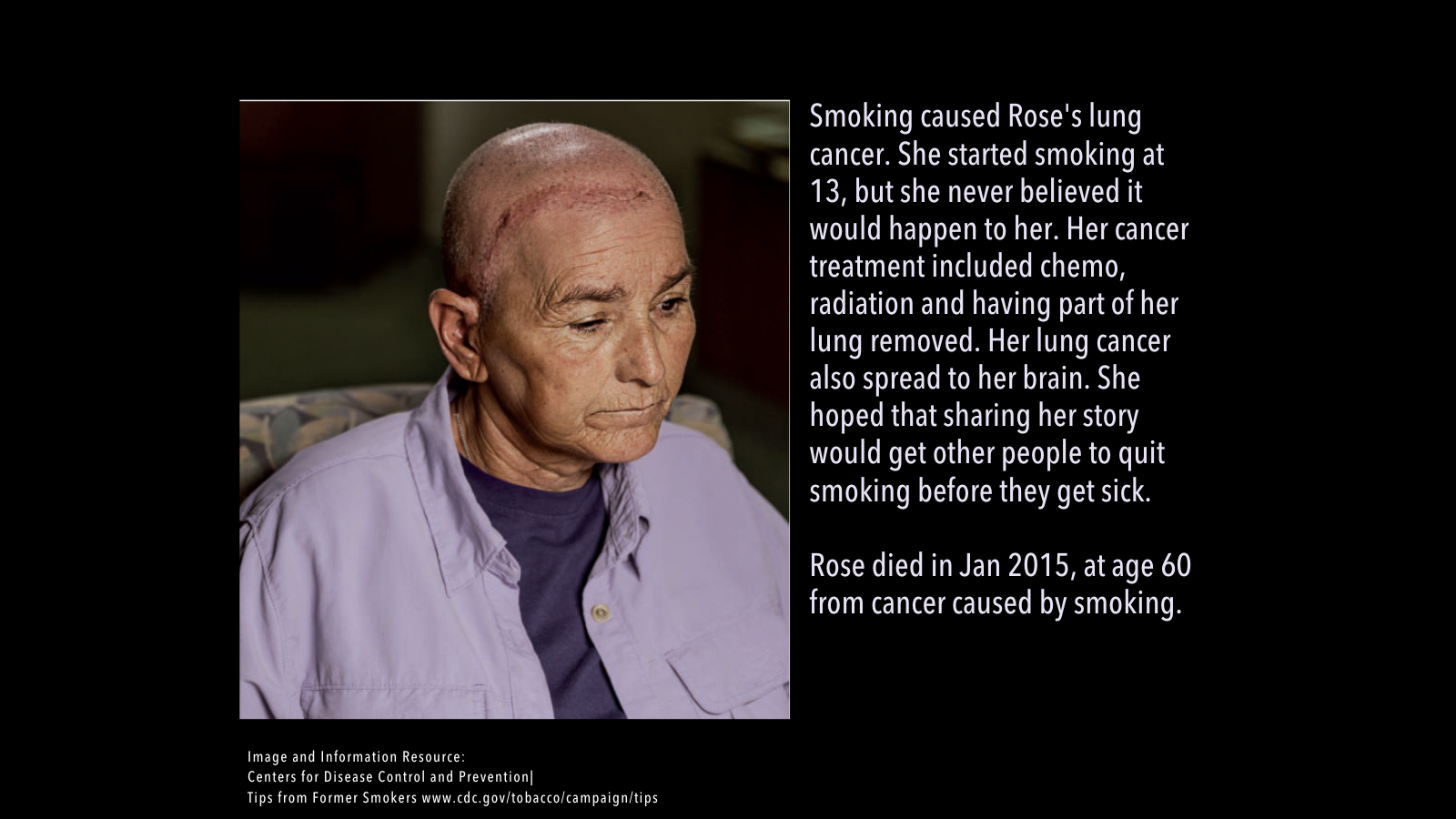
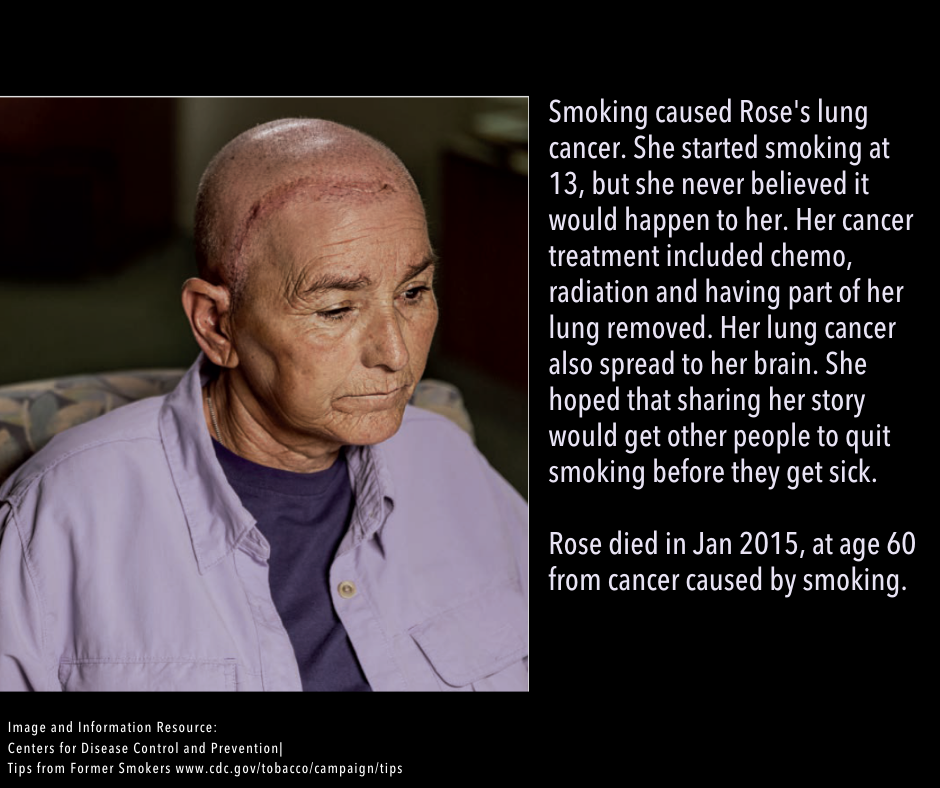
Learn from Rose, who developed #lungcancer from #smoking and needed very difficult treatments to treat her cancer: http://bit.ly/2a04qRs #CDCTips |
|
|
Learn about lung cancer screening and if it’s right for you with this guide from @theNCI: http://bit.ly/2a01T9K |
|
|
Breaking the stigma around #lungcancer starts with us. Learn more: https://bit.ly/3lBud9S #LCSM |

|
|
Thinking about quitting smoking? Let the #GreatAmericanSmokeout be your day to start your journey toward a smoke-free life http://bit.ly/2RtTNfM |

|
|
Tobacco hurts the LGBT community and kills more people in the U.S. than AIDS, alcohol, car accidents, homicide, suicide, illegal drugs, and fires combined. Learn more from FDA’s @ThisFreeLife Campaign: http://bit.ly/2a8wYak |

|
|
A #lungcancer diagnosis can be overwhelming. Here are some questions to ask your doc to help you understand your options: http://bit.ly/2Pd54iR |
|
|
Every #lungcancer patient & caregiver needs a guide. Access resources to get you on the right track: https://rb.gy/yggwss |

|
|
The Cancer Information Service from @TheNCI helps patients, health care professionals, friends and family get cancer information in English or Spanish. The service can also help you quit smoking. Chat, call or email today: http://bit.ly/2LkhvZM #LCSM #CompCancer |
|
|
African American men have the highest rates of lung cancer in the U.S. Lung cancers are mostly caused by smoking. For help quitting text QUIT to 47848 or visit www.smokefree.gov. http://bit.ly/2jQE2mm |
|
|
Knowing your family history of #lungcancer is important. Your risk may be higher if your family had lung cancer: http://bit.ly/2aeTTql |
|
|
Yearly screening with low-dose CT is recommended for people who meet certain eligibility criteria. Talk to your doctor about whether you should get screened for lung cancer: http://bit.ly/2xTd0zm |
|
|
Cancer doesn't wait and neither should you. Routine cancer screening is important, even during a pandemic. |
|
- How to post on Facebook
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select "Copy."
- Open Facebook. If you aren't already logged in, enter your email address (or phone number) and password, then tap "Log in."
- Tap the post box. This box is at the top of the News Feed. If you're posting to a group, you'll find the box just below the cover photo. There will generally be a phrase like "Write something" or "What's on your mind?" in the box.
- Tap "Photo/Video" near the middle of the post screen, then select the downloaded graphic to upload and tap "Done." Doing so adds the photo to your post.
- Tap "Post." It's in the top-right corner of the screen from the app, or the bottom-right from your computer. Doing so will create your post and add it to the page you're on.
| Message | Suggested Graphic |
| November is Lung Cancer Awareness Month. The most important things you can do to lower your lung cancer risk are to not smoke, quit smoking and avoid secondhand smoke. For free help quitting, visit smokefree.gov, call 1 (800) QUIT-NOW (784-8669) or text “QUIT” to 47848 from your cell phone. Find out more: http://bit.ly/2OS74wV |

|
| Tobacco use remains the single largest preventable cause of illness and death in the U.S. Get the facts as we kick off Lung Cancer Awareness Month: http://bit.ly/2xW3trc |
|
| In the U.S., about 41,000 people die each year from secondhand smoke-related diseases. Get more facts from the Truth Initiative here: http://bit.ly/2asftHJ |
|
| Radon is a cancer-causing, radioactive gas. You can't see, smell or taste radon but it may be a problem in your home. Get your home tested: http://bit.ly/2wxvd2u |
|
| Rose’s story highlights the dangers of smoking and its connection to lung cancer. Learn more by watching a video about the very difficult treatments needed to treat her cancer: https://bit.ly/3FBLgjQ |
|
| Is lung cancer screening right for you? Talk to your provider for more information and start with this helpful guide from the National Cancer Institute: http://bit.ly/2a01T9K |
|
| Lung cancer survivors are often socially stigmatized by friends or family members. End the silence and the stigma today. Here are some practical tips: https://bit.ly/3lBud9S |

|
| Today is the Great American Smokeout! Quitting smoking improves health immediately and over the long term. Let today be your day to start your journey toward a smoke-free life http://bit.ly/2RtTNfM |

|
| Tobacco hurts the LGBT community and kills more people in the U.S. than AIDS, alcohol, car accidents, homicide, suicide, illegal drugs and fires combined. Learn more from FDA’s This Free Life Campaign: http://bit.ly/2a8wYak |

|
| Being diagnosed with lung cancer can be overwhelming for patients and caregivers. Here are some questions to ask your doctor to help you understand the diagnosis and options to make decisions that are right for you or a loved one: http://bit.ly/2Pd54iR |
|
| Specialists at NCI’s Cancer Information Service can help patients, health care professionals, friends and family find cancer information in English and Spanish. The service can also help you quit smoking. Reach out by chat, call or email: http://bit.ly/2LkhvZM #CompCancer |
|
| Getting news of a lung cancer diagnosis is difficult, whether you’re a patient, loved one or a caregiver. Use this resource as a guide through your lung cancer journey for you and your loved ones: https://rb.gy/yggwss |

|
| African American men have the highest rates of lung cancer in the U.S. It’s never too late to quit smoking. Your risk for lung cancer goes down when you quit, no matter how old you are or how long you have smoked: http://bit.ly/2jQE2mm |
|
| New studies have shown that low-dose CT screening may be appropriate for people with high risk of lung cancer who meet certain eligibility criteria. Talk to your doctor about whether you should get screened for lung cancer: https://bit.ly/3FC4w0R |
|
| Having a parent, brother or sister or children who have had lung cancer may increase your risk. Learn more about family history and other risk factors from CDC: http://bit.ly/2aeTTql |
|
| Cancer doesn’t wait for COVID-19. Don’t put off preventive care, like lung cancer screening, to detect #lungcancer. It could save your life, so talk to your doctor today. |
|
- How to Post on LinkedIn
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select "Copy."
- Open LinkedIn. If you aren't already logged in, enter your email address and password, then tap "Log in."
- Tap "Start a post" from the main share box. This box is at the top of your profile.
- Tap "Photo" from the top of the post screen, then select the downloaded graphic to upload and tap "Done." Doing so adds the photo to your post.
- Tap "Post." It's in the the bottom-right. Doing so will create your post and add it to the page you're on.
| Message | Suggested Graphic |
| Early detection by screening is an important strategy for patients with an elevated risk of lung cancer. Providers: You may see patients in your office every day who could benefit from lung cancer screening. Check out this commentary by Dr. Lisa Richardson, Director of CDC’s Division of Cancer Prevention and Control to learn more: https://wb.md/2Pi5ViD |

|
| Providers: Check out this resource from the Centers for Disease Control and Prevention which compares guidelines and recommendations from several organizations regarding groups eligible for lung cancer screening: https://rb.gy/5saioo |

|
| Providers: Use the AHRQ clinician’s checklist to stay updated on lung cancer screening guidelines, how to evaluate patient eligibility for screening, and understand the importance of shared decision making. |
|
| Providers: Looking for more information on lung cancer prevention? Learn about who is at risk for lung cancer and interventions associated with a decreased risk of lung cancer with this PDQ cancer information summary from the National Cancer Institute: http://bit.ly/2MquGLN |

|
| Late diagnosis and stigma impact lung cancer survival rates. This fact sheet from SelfMade Health Network examines lung cancer diagnosis, survivorship, stigma, and its effect on nonsmokers: https://bit.ly/3v6ObMB |
|
| Providers: Do your patients know that nonsmokers are also at risk for lung cancer? Know the symptoms: https://bit.ly/3EpKepR |

|
| Providers: Cancer doesn’t wait for COVID-19. If eligible, remind your patients about preventive care, like lung cancer screening, to detect #lungcancer. It could save their life. |
|
- How to Post on Instagram
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select "Copy."
- Open Instagram. If you aren't already logged in, enter your username (or phone number) and password, then tap "Log in."
- Tap the plus sign box. This box is at the top right. Select the downloaded graphic or drag it into the box to upload it.
- Select "Square (1:1)" for the aspect ratio, then click "Next."
- Ignore the filters screen, then click "Next" again.
- Paste the caption where it says, "Write a caption..." at the top.
- Under "Accessibility," consider adding alt text to describe the photo for people with visual impairments.
- Tap "Share." It's in the bottom-right corner of the screen.
Download All Messages and Graphics
Social media management tools like Hootsuite and Sprout Social offer bulk scheduling options for uploading multiple messages at once. The spreadsheets below can be adapted to fit multiple scheduling platforms or services. They are currently formatted to work with Sprout Social's bulk scheduling option. Please review the bulk scheduling format requirements for your specific platform before posting. Messages are sorted by network.
Download All Facebook Messages
Download All LinkedIn Messages
Download All Instagram Messages
If you would like to download all images in this social media toolkit, click on each network below for a zip file with each network's graphics. Please note that these image sizes are slightly smaller than the links above due to file size limitations. If you would like to download full resolution versions, simply click on the "Download Graphic" link below each image in the message tables above.
Download All Facebook Graphics
Download All LinkedIn Graphics
Download All Instagram Graphics
References
American Cancer Society (2019). Cancer Facts & Figures for African Americans 2019-2021. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-african-americans/cancer-facts-and-figures-for-african-americans-2019-2021.pdf
American College of Surgeons (2020). Optimal Resources for Cancer Care: 2020 Standards. Retrieved from https://www.facs.org/-/media/files/quality-programs/cancer/coc/optimal_resources_for_cancer_care_2020_standards.ashx
American Lung Association (2020). State of Lung Cancer 2020: Racial and Ethnic Disparities. Retrieved from https://www.lung.org/research/state-of-lung-cancer/racial-and-ethnic-disparities
Arem, H., Mama, S. K., Duan, X., Rowland, J. H., Bellizzi, K. M., & Ehlers, D. K. (2020). Prevalence of healthy behaviors among cancer survivors in the United States: How far have we come? Cancer Epidemiology, Biomarkers & Prevention, 29(6), 1179–1187. https://doi.org/10.1158/1055-9965.EPI-19-131
Asian Pacific Partners for Empowerment, Advocacy, and Leadership (2019). Lung Cancer in Asian American, Native Hawaiian, and Pacific Islander Communities. Retrieved from https://appealforhealth.org/wp-content/uploads/2019/09/AANHPI-Lung-Cancer-Fact-Sheet-_Final.pdf
Boudreau, G., Hernandez, C., Hoffer, D., Preuss, K. S., Tibetts-Barto, L., Villaluz, N. T., & Scott, S. (2016). Why the World Will Never Be Tobacco-Free: Reframing "Tobacco Control" Into a Traditional Tobacco Movement. American Journal of Public Health, 106(7), 1188–1195.
Carter-Harris L., Hermann C.P., Schreiber J., Weaver M.T., & Rawl S.M. (2014). Lung Cancer Stigma Predicts Timing of Medical Help–Seeking Behavior. Oncol Nurs Forum, 41(3), E203-E210.
Centers for Disease Control and Prevention (2015). CDC Social Media Tools. Retrieved from http://www.cdc.gov/socialmedia/tools/index.html
Centers for Disease Control and Prevention (2019). Lung Cancer Incidence in the American Indian and Alaska Native Population, United States Purchased/Referred Care Delivery Areas—2012–2016 (U.S. Cancer Statistics data brief, no 14). Retrieved from Lung Cancer Incidence in the American Indian and Alaska Native Population, United States Purchased/Referred Care Delivery Areas—2012–2016 (cdc.gov)
Centers for Disease Control and Prevention (2020). Lung Cancer Statistics. Retrieved from https://www.cdc.gov/cancer/lung/statistics/
Centers for Disease Control and Prevention (n.d). Lung Cancer Among People Who Never Smoked. Retrieved from https://www.cdc.gov/cancer/lung/nonsmokers/index.htm
Centers for Disease Control and Prevention (n.d.). Social Determinants of Health. Retrieved from https://www.cdc.gov/chronicdisease/programs-impact/sdoh.htm
Centers for Disease Control and Prevention (n.d). What Are the Risk Factors for Lung Cancer? Retrieved from https://www.cdc.gov/cancer/lung/basic_info/risk_factors.htm
Centers for Disease Control and Prevention (n.d.). Who Should Be Screened for Lung Cancer? Retrieved from https://www.cdc.gov/cancer/lung/basic_info/screening.htm
Chae, J. (2016). Who Avoids Cancer Information? Examining a Psychological Process Leading to Cancer Information Avoidance. Journal of Health Communication, 21(7), 837–844. https://doi.org/10.1080/10810730.2016.1177144https://doi.org/10.1080/10810730.2016.1177144
Chae, J., Lee, C., Jensen, J.D. (2015). Correlates of cancer information overload: Focusing on individual ability and motivation. Health Communication, 31(5), 626-634. http://dx.doi.org/10.1080/10410236.2014.986026
Epstein, R.M., Street, R.L. (2007). A patient-centered approach to cancer communication research. In Patient-centered communication in cancer care: Promoting healing and reducing suffering (pp. 1-16). Bethesda, MD: National Cancer Institute.
Hamann, H. A., Ver Hoeve, E. S., Carter-Harris, L., Studts, J. L., & Ostroff, J. S. (2018). Multilevel Opportunities to Address Lung Cancer Stigma across the Cancer Control Continuum. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer, 13(8), 1062–1075. https://doi.org/10.1016/j.jtho.2018.05.014
Kanwal, M., Ding, X. & Cao, Y. (2017). Familial risk for lung cancer. Oncology Letters, 13(2), 525-542. doi: 10.3892/ol.2016.5518
Mekuria, A. B., Erku, D. A., & Belachew, S. A. (2016). Preferred information sources and needs of cancer patients on disease symptoms and management: A cross-sectional study. Patient Preference and Adherence, 10, 1991–1997. https://doi.org/10.2147/PPA.S116463
Miller, K.D., Ortiz, A.P., Pinheiro, P.S., Bandi, P., Minihan, A., Fuchs, H.E., Martinez Tyson, D., Tortolero-Luna, G., Fedewa, S.A., Jemal, A.M., Siegel, R.L. (2021) Cancer statistics for the US Hispanic/Latino population, 2021. CA Cancer J Clin. https://doi.org/10.3322/caac.21695
Mitchell, J. A., Williams, E.-D. G., Li, Y., & Tarraf, W. (2020). Identifying disparities in patient-centered care experiences between non-Latino white and black men: Results from the 2008-2016 Medical Expenditure Panel Survey. BMC Health Services Research, 20(1), 495–495. https://doi.org/10.1186/s12913-020-05357-5
National Cancer Institute. (2020). Cancer disparities. Retrieved August 11, 2021 from https://www.cancer.gov/about-cancer/understanding/disparities
National Native Network (n.d.). Cancer Prevalence. Retrieved from https://keepitsacred.itcmi.org/cancer/cancer-prevalence/
National Native Network (n.d.). Traditional vs. Commercial Tobacco. Retrieved from https://keepitsacred.itcmi.org/tobacco-and-tradition/traditional-v-commercial/
Quaife, S.L., Marlow, L.A., McEwen, A., Janes, S.M., Wardle, J. (2016). Attitudes toward lung cancer screening in socioeconomically deprived and heavy smoking communities: Informing screening communication. Health Expectations [Online ahead of print], 1-11. doi: 10.1111/hex.12481
Sullivan, D. R., Chan, B., Lapidus, J. A., Ganzini, L., Hansen, L., Carney, P. A., Fromme, E. K., Marino, M., Golden, S. E., Vranas, K. C., & Slatore, C. G. (2019). Association of Early Palliative Care Use With Survival and Place of Death Among Patients With Advanced Lung Cancer Receiving Care in the Veterans Health Administration. JAMA oncology, 5(12), 1702–1709. https://doi-org.proxygw.wrlc.org/10.1001/jamaoncol.2019.3105
The Center for Black Health and Equity (n.d.). African Americans and Cancer. Retrieved from https://centerforblackhealth.org/cancer/
Torre, L. A., Sauer, A. M., Chen, M. S., Jr, Kagawa-Singer, M., Jemal, A., & Siegel, R. L. (2016). Cancer statistics for Asian Americans, Native Hawaiians, and Pacific Islanders, 2016: Converging incidence in males and females. CA: A Cancer Journal for Clinicians, 66(3), 182–202. https://doi.org/10.3322/caac.21335
Underwood, J.M. (2014, July 29). Lung Cancer Burden among the American Indian and Alaska Native Populations. National Native Network. http://keepitsacred.itcmi.org/wp-content/uploads/sites/5/2015/06/Underwood.NNN_.pdf
Underwood, J.M., Townsend, J.S., Stewart, S.L., Buchannan, N., Ekwueme, D.U., Haskins, N.A….Fairley, T.L. (2012). Surveillance of demographic characteristics and health behaviors among adult cancer survivors – Behavioral Risk Factor Surveillance System, United States, 2009. Morbidity and Mortality Weekly Report, 61(SS01), 1-23. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/ss6101a1.htm
U.S. Cancer Statistics Working Group, Centers for Disease Control and Prevention. (2021). Cancer statistics data visualization tool, basd on 2020 submission data (1999-2018). Retrieved August 6, 2021 from https://gis.cdc.gov/Cancer/USCS/#/AtAGlance
White-Means, S., and Osmani, A. R. (2017). Racial and ethnic disparities in patient-provider communication with breast cancer patients: Evidence from 2011 MEPS and experiences with cancer supplement. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, 54, 1-17. https://doi.org/10.1177/0046958017727104
Williamson, T. J., Rawl, S. M., Kale, M. S., & Carter-Harris, L. (2021). Lung cancer screening and stigma: Do smoking-related differences in perceived lung cancer stigma emerge prior to diagnosis? Stigma and Health. https://doi-org.proxygw.wrlc.org/10.1037/sah0000300.supp (Supplemental)