Palliative Care
Palliative care, sometimes called supportive or comfort care, is a type of comprehensive medical care for people diagnosed with a serious illness. Palliative care is focused on relieving and preventing physical, emotional and social side effects caused by illness or curative treatments.1 Palliative care may be given in the hospital, at home, at an outpatient clinic or at a long-term care facility. Palliative care can be administered to patients of all ages and at any stage of disease, and is not the same as end-of-life or hospice care.1 Unlike hospice care, which is usually administered when the goal is no longer to cure the illness, palliative care can be given in conjunction with curative treatment and can be initiated as soon as the disease is diagnosed.1
Data and Statistics
The American Society of Clinical Oncology (ACSO) encourages the integration of palliative care services for patients with advanced cancer into all standard oncology practices.2 Research shows that patients with cancer who receive palliative care report improved mood, health care utilization, quality of life, and patient satisfaction.3 Some research also showed prolonged survival for patients with metastatic non-small cell lung cancer who received palliative care concurrently with cancer treatments, compared to patients who received cancer treatments alone.4
When and how palliative care is provided can make a significant difference in health outcomes. According to one study, interdisciplinary specialist palliative care in stand-alone clinics remains the gold standard for ambulatory palliative care because this approach has the greatest impact on multiple patient and caregiver outcomes.32 Despite this finding, palliative care is still inaccessible for many patients due to variety of reasons.
Globally, The World Health Organization (WHO) estimates that only 14% of people who need palliative care receive these services.5 In the U.S., 72% of U.S. hospitals with 50 or more beds report having a palliative care program, and 94% of hospitals with 300 or more beds have a dedicated palliative care team.6 However, over 80% of health institutions in the US with palliative care programs report insufficient capacity to meet increasing demands.3 Access to palliative care is especially limited in rural areas, with only 17% of rural hospitals in the U.S. reporting palliative care programs.5
In addition to lack of access to palliative care, there is still confusion about its purpose. A 2020 study revealed that only 29% of U.S. adults know about palliative care, and among them, 87% had misconceptions about it.7 The most common misconceptions were automatically associating palliative care with death (44%), equating palliative care with hospice (38%), believing palliative care could not be concurrent with treatments (18%), and seeing palliative care as “giving up” (16%).7
Analysis of the National Cancer Institute's Health Information National Trends Survey revealed that among cancer survivors, 66% reported no knowledge of palliative care, 18% knew a little, and only 17% were able to explain palliative care to someone else.8 However, cancer survivors who reported existing knowledge of palliative care had fewer misconceptions and were less likely to associate palliative care with death, hospice care or giving up.8 A separate multivariable analysis indicated that cancer survivors of color are significantly less likely to report knowledge of palliative care.9
Another study of the knowledge of palliative care in the U.S. general population showed that self-identified white women have greater odds of being more aware of palliative care. Those reporting Hispanic ethnicity had lower odds.33 That same study suggests that some racial minorities underuse palliative care even with sufficient access; this might be due to communication barriers, lack of trust in the health care system, and lack of insurance coverage or limited reimbursement. These data suggest there is limited awareness of palliative care in the United States, despite its documented benefits. Addressing this awareness gap is a priority to change norms around using palliative care services. Community- and population-based interventions are necessary to raise awareness and inform the public about palliative care.
Best Practices for Communicating About Palliative Care
- Increase knowledge and awareness about palliative services and benefits.
-
- Health care providers and comprehensive cancer control professionals should share general information and resources to increase awareness of palliative care and reduce misunderstanding. Lack of awareness and communication between provider and patients is a foremost barrier to timely referrals to palliative care.10
- Highlight the physical, emotional, spiritual and practical benefits of palliative care for patients.2
- Public health professionals can share resources that providers can give patients to further inform them of palliative care’s meaning and benefits.
- Highlight the potential of palliative care to reduce medical costs for patients. Research shows that beginning palliative care within three days of admission reduces overall cost for all hospitalized adults, with even greater savings shown for patients with cancer.11
- Acknowledge the needs of palliative caregivers and share resources to support their well-being.
- Encourage policy, system and environmental (PSE) changes to support caregivers of patients receiving at-home palliative care. Globally, caregivers encounter significant barriers to balancing patient support and their own employment.12
- Public health professionals should share examples of effective PSE changes that other health systems can use to guide their own palliative care efforts.
- Public health professionals should promote two-way communication about palliative care that acknowledges patient values.
- Correct misunderstanding and myths about palliative care
-
- Clarify the difference between palliative and hospice care and separate the terms, which can help to increase frequency of provider referrals for palliative care. Research shows that many physicians did not refer patients to palliative care because they referred them to hospice instead, misleading individuals that palliative care is for patients with limited life expectancy rather than for the broader population of severely ill patients.13
- Remind providers to refer patients to palliative care services at the time of diagnosis or when treatment begins, as later referrals could contribute to associating palliative care with end-of-life care.14
- Challenge the misunderstanding that palliative care is only for elderly and end-of-life patients by highlighting patients of different ages, backgrounds and health statuses receiving care.
- Share messages that remind patients and providers that palliative care can be administered at the same time as cancer treatments.
- Explain the purpose and scope of palliative care services to the patient and caregivers. Provide examples to demonstrate the differences between palliative care and hospice care.
- Ease concerns and challenge stigmas about pain management in palliative care
-
- Promote palliative care as a resource for navigating pain management for patients diagnosed with cancer. Worry about addiction and fear of stigma are becoming increasingly common for cancer survivors who are prescribed opioids as part of their symptom management; however, conversations with providers are shown to help relieve worries.15
- Promote palliative care as a resource for providers to connect cancer survivors with pain management expertise. Research shows that some providers who do not feel they have adequate training or experience with pain management have turned to palliative care teams to optimize pain management regimens.15
- Acknowledge commonly cited barriers to integrating palliative care into cancer care
-
- Encourage health systems and clinics to designate leaders who can guide palliative care training within their programs, as well as help staff make time for palliative care efforts. Oncology professionals frequently identify a lack of senior palliative care leadership or administration as a main challenge to integrating palliative care best practices.16
Communicating with Subgroups
Communication-related issues may also play a role in health disparities and patient engagement. Consider the information most useful to each subgroup (see below for specific messaging and read more on health disparities here). Tailor communication to these priority populations with messages that also address conditions where these communities live, learn, work and play, as these social determinants of health can impact a wide range of health risks and outcomes. To ensure messages resonate with the intended audience, we also recommend referring to the National Networks’ existing resources and adapting messages to reflect individuals with lived experiences.
- Black/African American Persons
-
- Remind providers to refer Black patients with cancer to palliative services, as research shows that non-Hispanic Black patients are less likely to receive palliative care services in hospital settings than non-Hispanic White patients.18 Black persons diagnosed with advanced cancers are also less likely to receive a palliative care consultation after being discharged from the hospital.18
- Encourage providers to distribute educational materials to help Black caregivers manage care responsibilities and financial burdens. Non-Hispanic Black caregivers are shown to experience higher levels of caregiving intensity and financial hardship than non-Hispanic White caregivers.34
- Tell providers to consider using faith- and community-based interventions, as research suggests this may increase participation of non-Hispanic Black patients in palliative care and may encourage completion of advance care directives, which are legal documents that provide instruction for medical care in the case one cannot communicate their wishes.35
- LGBTQI+ Persons
-
- Create messages that help health providers recognize and overcome implicit bias when discussing palliative care with patients. LGBTQI+ patients and survivors report fears of social stigma as well as experiencing stigma within health care settings.19 Addressing implicit bias may help to reduce stigma and to foster patient trust and honesty.
- Remind providers of best practices for communicating with LGBTQI+ patients and share tips for creating a welcoming environment. A survey of healthcare professionals revealed that 15.6% observed disrespectful or inadequate palliative care for LGBTQI+ patients,20 and 21.3% observed disrespectful or inadequate care for transgender patients.21
- Hispanic/Latino/a/x Persons
-
- Encourage providers to create and share resources featuring Hispanic and Latino/a/x role models, such as brief palliative care introductory videos. A research study found that after viewing a four-minute video featuring a Spanish-speaking palliative care patient, hospitalized Hispanic and Latino/a/x adults were more likely to enroll themselves and/or family members in palliative care.22
- Share multilingual resources, as removing language barriers is shown to improve access to quality care for Hispanic and Latino/a/x patients.23 If providers use translators, remind them that translators should not be the patient’s relatives.24
- AANHPI (Asian American, Native Hawaiian/Pacific Islander) Persons
-
- Remind providers of factors that may affect AANHPI people’s decisions about or access to palliative care. Individual level barriers may include lack of knowledge about palliative care, the preference and/or cultural practice for family-based decision making, language barriers and cultural beliefs.25
- Instruct providers to refer AANHPI patients with cancer to clinical trials, as this demographic is underrepresented in palliative care research.25
- AI/AN (American Indian, Alaska Native) Persons
-
- Craft messages informed by the lived experiences of AI/AN cancer survivors, spiritual leaders, and community and ceremonial elders to demonstrate cultural competency in care practices. For some AI/AN patients, spiritual care may be just as important as physical and mental components of care.26 Factors such as separation from family and tribal communities can leave patients feeling spiritually vulnerable and may deter patients from seeking or continuing palliative care.
- Share messages that engage providers in raising awareness of palliative care among AI/AN individuals. A study of 270 AI/AN elders found that none had heard of palliative care.27
- Rural
-
- Encourage providers to lead educational sessions on palliative care with staff members to reduce misconceptions within the healthcare setting. A study of rural health organizations revealed that a lack of clinician knowledge and experience is a main obstacle to creating impactful palliative care teams.28 Other cited barriers were lack of community awareness, lack of reimbursement or funding strategies, coordination of care between providers and medical staff commitment.28
- Share resources that providers can distribute to patients and their families. Some rural patients and families reported difficulty reaching their palliative care providers or accessing basic information.29 Poor health literacy was also a factor, indicating a need for accessible, easy-to-understand resources.29 However, providers reported a lack of available resources to share with patients.29
- Promote the use of telehealth technologies to reach patients located in rural or remote locations.30 While not all aspects of care can be provided virtually, telehealth communications can be effective for patient and medication monitoring, specialist appointments and palliative care consultations.30
- Socioeconomic status (SES)
-
- Distribute financial information and resources for cancer survivors with lower incomes. Research shows that patients with low income are less likely to receive specialized palliative care than patients with more income and higher levels of education.31 See “Palliative Care Resources” below for a selection of organizations offering financial aid to patients with cancer.
Palliative Care Messages and Graphics
Download All Messages and Graphics How to Post on Social Media
|
Topics |
Suggested Images |
|---|---|
|
Topic: Clearly define palliative use and its benefits #cdc #dcpc #cctpalliative |

|
|
Topic: Highlight the global underutilization of palliative care services #cdc #dcpc #cctpalliative |
|
|
Topic: Explain the difference between palliative care and hospice/end-of-life care #cdc #dcpc #cctpalliative |

|
|
Topic: Help palliative care teams understand the needs of diverse demographics #cdc #dcpc #cctpalliative #healthequity |

|
|
Topic: Share resources to support palliative caregivers of family members with cancer #cdc #dcpc #cctpalliative #caregiving |
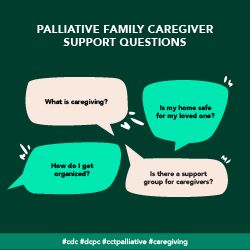
|
|
Topic: Provide multilingual resources with basic palliative care information #cdc #dcpc #cctpalliative #hispanichealth |

|
|
Topic: Share examples of effective PSE changes #cdc #dcpc #cctpalliative |

|
|
Topic: Remind providers to start palliative care at the time of diagnosis #cdc #dcpc #cctpalliative |

|
|
Topic: Creating a welcoming environment for LGBTQI+ patients #cdc #dcpc #cctpalliative #lgbthealth |
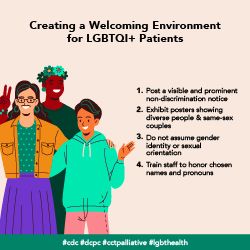
|
|
Topic: Providing inclusive care for transgender patients #cdc #dcpc #cctpalliative #transhealth |
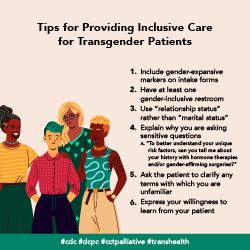
|
|
Topic: Promote the use of telehealth services to administer certain aspects of palliative care to rurally located patients #cdc #dcpc #cctpalliative |

|
|
Topic: Distribute financial information and resources to offset costs of palliative care #cdc #dcpc #cctpalliative |

|
|
Topic: Encourage providers to participate in insurance plans with high coverage #cdc #dcpc #cctpalliative |

|
Download All Messages and Graphics How to Post on Social Media
How to Post to Social Media
Start by downloading the ZIP file above. Then double click the downloaded file to unzip and open the folder. Inside, you’ll find three CSV files.
- Messaging.csv contains captions for all messages in the toolkit, organized by topic.
- Bulk - Instagram.csv contains captions for all Instagram messages, along with graphics URLs that can be used to bulk schedule both text and images.
- Bulk - LinkedIn-Facebook.csv contains captions for all LinkedIn, Facebook, and Twitter messages, along with graphics URLs that can be used to bulk schedule both text and images.
- Bulk - Twitter.csv contains captions for all Twitter messages, along with graphics URLs that can be used to bulk schedule both text and images.
Inside the main folder, you’ll also see two sub-folders containing the messaging graphics for all major platforms. The first folder contains rectangular images suited for use on Facebook, Twitter, and LinkedIn. The second folder contains square images suited for Instagram.
Select your platform below for additional instructions.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Facebook. If you aren’t already logged in, enter your email address (or phone number) and password, then tap “Log in.”
- Tap the post box. This box is at the top of the News Feed. If you're posting to a group, you’ll find the box just below the cover photo. There will generally be a phrase like “Write something”or “What’s on your mind?” in the box.
- Tap “Photo/Video” near the middle of the post screen, then select the downloaded graphic to upload and tap “Done.” Doing so adds the photo to your post.
- Tap “Post.” It’s in the top-right corner of the screen from the app, or the bottom-right from your computer. Doing so will create your post and add it to the page you’re on.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Twitter. If you aren’t already logged in, enter your email address and password, then tap “Log in.”
- Tap the post button. This button is at the bottom right of the News Feed. There will generally be a phrase like “What’s happening?” in the box.
- Tap the camera icon near the middle of the post screen, or the picture icon in the bottom left of the post screen then select the downloaded graphic to upload, and add the post caption.
- Tap “Tweet.” It’s in the top-right corner of the screen from the app, or the bottom-right from your computer. Doing so will create your post and add it to the page you’re on.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Instagram. If you aren’t already logged in, enter your username (or phone number) and password, then tap “Log in.”
- Tap the plus sign box. This box is at the top right. Select the downloaded graphic or drag it into the box to upload it.
- Select “Square (1:1)” for the aspect ratio, then click “Next.”
- Ignore the filters screen, then click “Next” again.
- Paste the caption where it says, “Write a caption…” at the top.
- Under “Accessibility,” consider adding alt text to describe the photo for people with visual impairments.
- Tap “Share.” It's in the bottom-right corner of the screen.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open LinkedIn. If you aren’t already logged in, enter your email address and password, then tap “Log in.”
- Tap “Start a post” from the main share box. This box is at the top of your profile.
- Tap “Photo” from the top of the post screen, then select the downloaded graphic to upload and tap “Done.” Doing so adds the photo to your post.
- Tap “Post.” It's in the the bottom-right. Doing so will create your post and add it to the page you’re on.
- Bulk Scheduling
-
Social media management tools like Hootsuite and Sprout Social offer bulk scheduling options for uploading multiple messages at once. The spreadsheets included in the download can be adapted to fit multiple scheduling platforms or services. They are currently formatted to work with Sprout Social’s bulk scheduling option. Please review the bulk scheduling format requirements for your specific platform before posting. Messages are sorted by network.
Palliative Care Resources
|
Resource |
Description |
|---|---|
| American Academy of Hospice and Palliative Care | A professional organization for physicians specializing in hospice and palliative medicine, nurses, and other healthcare providers. Its core mission is to expand access of patients and families to high-quality palliative care and advance the discipline of hospice and palliative medicine through professional education and training, development of a specialist workforce, support for clinical practice standards, and research and public policy. |
| CancerCare | A national organization providing free, professional support services and information to help people manage the emotional, practical and financial challenges of cancer. |
| CaringInfo | A program of the National Hospice and Palliative Care Organization that provides free resources to educate and empower patients and caregivers. |
| Center to Advance Palliative Care | CAPC is the leading resource for palliative care program development and growth. Access essential palliative care tools, education, resources and training for healthcare professionals. |
| ClinicalTrials.gov | A compendium of completed, recruiting, and upcoming clinical trials related to palliative care services. |
| Cancer Financial Assistance Coalition | A coalition of organizations helping cancer patients manage their financial challenges. |
| Get Palliative Care | A website providing clear, comprehensive palliative care information for people living with a serious illness. |
| International Palliative Care Resource Center | IPCRC is dedicated to making palliative care resources accessible for health care professionals, building palliative care capacity worldwide and providing a dynamic and constantly expanding website. |
| Leukemia & Lymphoma Society Patient Financial Assistance Programs | A series of programs offering financial assistance to patients diagnosed with blood cancers such as leukemia, lymphoma, or multiple myeloma. |
| Make it Your Own | A tool for helping medical professionals to create tailored health communications with evidence-based messaging and customized images. |
| National Cancer Institute | Review frequently asked questions and misconceptions about palliative care, and access resources for continued learning. |
| National Hospice and Palliative Care Organization | The nation’s largest membership organization for providers and professionals who care for people affected by serious and life-limiting illness. NHPCO gives ongoing inspiration, practical guidance, and legislative representation to hospice and palliative care providers so they can enrich experiences for patients and ease caregiving responsibilities and emotional stress for families. |
References
