National Minority Health Month and Minority Cancer Awareness Week
National Minority* Health Month (NMHM) is observed annually in April. NMHM is an opportunity to raise awareness about health disparities affecting populations that have been marginalized, discriminated against and excluded in American culture, both historically and currently. NMHM acknowledges the social, economic and geographic disadvantages that intersect across disability status, sexual orientation, gender identity, race and ethnicity, which have historically been linked to discrimination or exclusion.1
During NMHM, National Minority Cancer Awareness Week (NMCAW) provides a more specific opportunity to raise awareness about cancer-related health disparities.2
This health awareness social media toolkit is designed to help cancer control organizations implement evidence-based practices when communicating about National Minority Health Month, Minority Cancer Awareness Week and cancer prevention among marginalized communities.
*A note on language:
We use the word “minority” within this toolkit to align with the name of the awareness month. We otherwise discourage use of the term “minority” in awareness messaging, as it can wrongfully imply that racial and ethnic groups are outnumbered by non-Hispanic White Americans and can contribute to the perpetuation of stereotypes and implicit bias.3,4
The CDC reports: “According to the 2018 U.S. Census report, the year 2030 marks a demographic turning point for the United States. The nation’s population is projected to age considerably and become more racially and ethnically diverse. The population of people who are more than one race is projected to be the fastest growing racial or ethnic group over the next several decades, followed by Asian Americans and Hispanic/Latino Americans.”
Best Practices for Communicating About NMHM & NMCAW
Recognize cultural differences and values, as cultural background significantly impacts the lens through which people view health information.
-
- Learn from your intended to optimize culturally appropriate messaging and communication channels.
- Incorporate cultural norms, values and religious beliefs into health messages, rather than surface-level cultural features, such as risk statistics of a particular group.5
- Integrate cross-cultural knowledge into messages. This means learning from people within your intended audience and understanding stresses caused by politics or laws.6
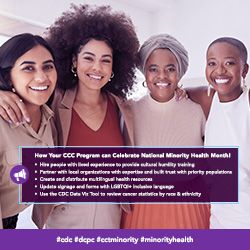
- Promote cultural humility among providers and staff. Cultural humility refers to the willingness to honor cultural beliefs, engage in self-reflection and continue learning.7 Cultural competency is a misnomer that assumes one can learn once and for all about people who have different lived experiences from their own.7
Use plain language and narrative to communicate culturally relevant messages.
-
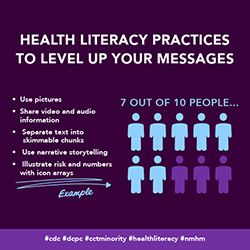
- Reduce the health literacy level of messages. Low health literacy is associated with poorer health outcomes and lack of participation in cancer screening programs.8
- Keep messages concise and use plain language. The use of plain language makes messaging accessible to more people in a shorter amount of time.9 Reference these CDC guidelines for making language accessible and understandable.5
- Provide health information in languages appropriate for the intended audience.10 Multilingual messages should be crafted and reviewed by people with lived experiences shared by your populations of focus.11
- Make messages accessible to people with disabilities by using braille, American Sign Language, large print text, closed captioning, audio descriptions and plain language.12
- Use narratives to improve learner comprehension and recall.13 Narratives can help reach people who have had past negative experiences in health care.
- Use culturally appropriate health promotion messages to support behavior change.14
Point people to community resources.
-
- Promote community-based resources across the cancer continuum, including prevention, screening, treatment, and survivorship resources. Outreach, education and research are crucial for addressing health disparities.15
- Leverage partnerships with local media to increase knowledge and access to information across diverse communities.16
- Form community partnerships across other sectors,such as business, labor, civic/social, urban planners, education, transportation, housing and public safety. Partnerships with community-based organizations who serve priority populations can help healthcare organizations address structural bias in our systems.17
- Join existing movements and conversations (such as NMHM and NMCAW) to increase your reach. Use relevant hashtags to increase the reach of your messages.
Communicating with Diverse Audiences
Consider the information most useful for specific populations. Tailor communication to where these communities live, learn, work and play. Refer to and adapt the National Networks’ existing resources.
Consider the information most useful for specific populations. Tailor communication to the communities where populations of focus live, learn, work and play. Refer to and adapt the National Networks’ existing resources.
- Black/African American Persons
-
- Share information about cancer inequities affecting Black and African American people to raise awareness of symptoms, encourage screenings and promote healthier behaviors. For example:
- Black people experience the highest overall cancer mortality rates compared to other racial and ethnic groups.18
- Prostate cancer, female breast cancer, lung and bronchus cancer, and colon and rectum cancer are the most common cancers that occur among Black Americans.18
- Prostate cancer, lung and bronchus cancer, female breast cancer, and colon and rectum cancer cause the most cancer-related deaths among Black Americans.18
- HPV vaccination eliminates precancerous cells and saves lives, but Black Americans have lower vaccination rates than White Americans.19
- Share information about cancer inequities affecting Black and African American people to raise awareness of symptoms, encourage screenings and promote healthier behaviors. For example:
- LGBTQI+ Persons
-
- Share information about cancer inequities affecting LGBTQI+ people.
- Gay and bisexual men are at higher risk for anal cancer than heterosexual men.20
- Lesbian and bisexual women are at higher risk for breast cancer and certain gynecologic cancers than heterosexual women.20
- Transgender and gender-nonconforming people are less likely to receive cancer screenings that are appropriate for their organs.20
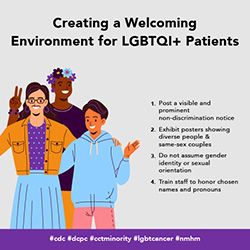
- Communicate the importance of culturally-affirming care.Stigma experienced by LGBTQI+ patients causes healthcare avoidance. 21Health providers are responsible for recognizing personal and structural bias and creating safe environments to optimize patient wellbeing.
- Highlight barriers to quality care and share resources to address them.
- Share resources like the National LGBT Cancer Network to help providers understand cancer-related health disparities among LGBTQI+ people.
- Share information about cancer inequities affecting LGBTQI+ people.
- Hispanic/Latino/a/x Persons
-
- Share information about cancer inequities affecting Hispanic and Latino/a/x people.
- Female breast cancer, prostate cancer, colon and rectum cancer, and lung and bronchus cancer are the most commonly occurring cancers among Hispanic and Latino/a/x persons.18
- Prostate cancer, lung and bronchus cancer, female breast cancer, and colon and rectum cancer cause the most cancer-related deaths among this population.18
- Hispanic and Latino/a/x people experience the second-highest death rates from lung cancer and liver cancer among all racial and ethnic groups.18
- Hispanic and Latino/a/x people experience the highest stomach cancer incidence and mortality rates.18
- Remind providers to communicate the risk of skin cancer, as Hispanic and Latino/a/x people are historically less likely than White peers to use sun protection.22
- Provide health information in Spanish. Research shows that people with Limited English Proficiency (LEP) are less likely to utilize health services.23
- Share information about cancer inequities affecting Hispanic and Latino/a/x people.
- AANHPI (Asian American, Native Hawaiian/Pacific Islander) Persons
-
- Share information about health inequities affecting AANHPI people.
- Female breast cancer, prostate cancer, lung and bronchus cancer, and colon and rectum cancer are the most commonly occurring cancers among AANHPI people.18
- Lung and bronchus cancer, female breast cancer, colon and rectum cancer, and prostate cancer cause the most cancer-related deaths among AANHPI people.18
- Disaggregate AANHPI subgroups and tailor messages to a specific subgroup.Cancer risk and incidence varies greatly between AANHPI subgroups and ethnicities.24,25
- Hmong people have a higher risk of prostate cancer compared to Chinese people.26 Kampuchean patients are less likely to receive treatment than Hmong or Hawaiian patients.26
- Incidence of oropharyngeal squamous cell carcinoma is higher among Native Hawaiian men than among Chinese men.27
- Incidence of cervical carcinoma is higher among Laotian women than among Asian Indian and Pakistani women.27
- Encourage the availability and distribution of health information in multiple Asian languages based on who lives in your catchment area.
- Share information about health inequities affecting AANHPI people.
- AI/AN (American Indian, Alaska Native) Persons
-
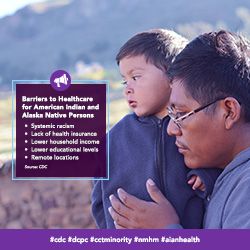
- Craft messages informed by the lived experiences of AI/AN cancer survivors, spiritual leaders, and community and ceremonial elders. Factors such as separation from family and tribal communities can leave patients feeling spiritually vulnerable and may deter patients from seeking or continuing care.28
- Share information about cancer inequities affecting AI/AN people.
- Female breast cancer, prostate cancer, lung and bronchus cancer, and colon and rectum cancer are the most commonly occurring cancers among AI/AN people.18
- Lung and bronchus cancer, female breast cancer, colon and rectum cancer, and prostate cancer cause the most cancer-related deaths among AI/AN people.18
- American Indians/Alaska Natives have the highest rates of liver and intrahepatic bile duct cancer.18
- Immigration Status
-
- Share information about cancer inequities and barriers to care affecting immigrant populations.
- Immigrants are less likely to receive screening tests for cervical, breast and colorectal cancers than the general U.S. population.29
- Language barriers and a lack of insurance may hinder use of health services and lead to worse health outcomes for immigrants.30
- Share information about cancer inequities and barriers to care affecting immigrant populations.
Sample Messages and Graphics
Download All Messages and Graphics How to Post on Social Media
|
Topics |
Suggested Images |
|---|---|
|
Topic: Engage providers in National Minority Health Month #cdc #dcpc #cctminority #minorityhealth |
|
|
Topic: Engage Providers in Minority Cancer Awareness Week #cdc #dcpc #cctminority #minorityhealth |

|
|
Topic: Share multilingual health resources #cdc #dcpc #cctminority #minorityhealth |
|
|
Topic: Tips for incorporating best health literacy practices in messaging #cdc #dcpc #cctminority #healthliteracy #nmhm |
|
|
Topic: Educate providers on LGBTQI+ people’s cancer risk #cdc #dcpc #cctminority #transhealth #nmhm |

|
|
Topic: Share information about sun safety #cdc #dcpc #cctminority #latinohealth #nmhm |

|
|
Topic: Highlight health inequities affecting Black & African American people #cdc #dcpc #cctminority #nmhm #blackhealth #pse |

|
|
Topic: Highlight health inequities affecting American Indians and Alaska Natives #cdc #dcpc #cctminority #nmhm #aianhealth |
|
|
Topic: Highlight health inequities affecting Asian Americans and Native Hawaiians/Pacific Islanders #cdc #dcpc #cctminority #nmhm #aanhpihealth |

|
|
Topic: Highlight health inequities affecting Hispanic and Latino/a/x people #cdc #dcpc #cctminority #latinohealth #nmhm |
|
|
Topic: Tips for caring for LGBTQI+ patients #cdc #dcpc #cctminority #lgbtcancer #nmhm |
|
|
Topic: Tips for caring for transgender patients #cdc #dcpc #cctminority #lgbtcancer #transhealth #nmhm |

|
|
Topic: Recommend prostate screenings for Black patients #cdc #dcpc #cctminority #blackhealth #nmhm |
|
|
Topic: Tips for creating cross-cultural messaging #cdc #dcpc #cctminority #nmhm |

|
|
Topic: Encourage cultural humility, not cultural competency #cdc #dcpc #cctminority |
|
|
Topic: Highlight information about adverse childhood experiences (ACEs) and cancer risk #cdc #dcpc #cctminority #nmhm #aces |

|
Download All Messages and Graphics How to Post on Social Media
How to Post to Social Media
Start by downloading the ZIP file above. Then double click the downloaded file to unzip and open the folder. Inside, you’ll find three CSV files.
- Messaging.csv contains captions for all messages in the toolkit, organized by topic.
- Bulk - Instagram.csv contains captions for all Instagram messages, along with graphics URLs that can be used to bulk schedule both text and images.
- Bulk - LinkedIn-Facebook.csv contains captions for all LinkedIn, Facebook, and Twitter messages, along with graphics URLs that can be used to bulk schedule both text and images.
- Bulk - Twitter.csv contains captions for all Twitter messages, along with graphics URLs that can be used to bulk schedule both text and images.
Inside the main folder, you’ll also see two sub-folders containing the messaging graphics for all major platforms. The first folder contains rectangular images suited for use on Facebook, Twitter, and LinkedIn. The second folder contains square images suited for Instagram.
Select your platform below for additional instructions.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Facebook. If you aren’t already logged in, enter your email address (or phone number) and password, then tap “Log in.”
- Tap the post box. This box is at the top of the News Feed. If you're posting to a group, you’ll find the box just below the cover photo. There will generally be a phrase like “Write something”or “What’s on your mind?” in the box.
- Tap “Photo/Video” near the middle of the post screen, then select the downloaded graphic to upload and tap “Done.” Doing so adds the photo to your post.
- Tap “Post.” It’s in the top-right corner of the screen from the app, or the bottom-right from your computer. Doing so will create your post and add it to the page you’re on.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Twitter. If you aren’t already logged in, enter your email address and password, then tap “Log in.”
- Tap the post button. This button is at the bottom right of the News Feed. There will generally be a phrase like “What’s happening?” in the box.
- Tap the camera icon near the middle of the post screen, or the picture icon in the bottom left of the post screen then select the downloaded graphic to upload, and add the post caption.
- Tap “Tweet.” It’s in the top-right corner of the screen from the app, or the bottom-right from your computer. Doing so will create your post and add it to the page you’re on.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Instagram. If you aren’t already logged in, enter your username (or phone number) and password, then tap “Log in.”
- Tap the plus sign box. This box is at the top right. Select the downloaded graphic or drag it into the box to upload it.
- Select “Square (1:1)” for the aspect ratio, then click “Next.”
- Ignore the filters screen, then click “Next” again.
- Paste the caption where it says, “Write a caption…” at the top.
- Under “Accessibility,” consider adding alt text to describe the photo for people with visual impairments.
- Tap “Share.” It's in the bottom-right corner of the screen.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open LinkedIn. If you aren’t already logged in, enter your email address and password, then tap “Log in.”
- Tap “Start a post” from the main share box. This box is at the top of your profile.
- Tap “Photo” from the top of the post screen, then select the downloaded graphic to upload and tap “Done.” Doing so adds the photo to your post.
- Tap “Post.” It's in the the bottom-right. Doing so will create your post and add it to the page you’re on.
- Bulk Scheduling
-
Social media management tools like Hootsuite and Sprout Social offer bulk scheduling options for uploading multiple messages at once. The spreadsheets included in the download can be adapted to fit multiple scheduling platforms or services. They are currently formatted to work with Sprout Social’s bulk scheduling option. Please review the bulk scheduling format requirements for your specific platform before posting. Messages are sorted by network.
Resources
|
Resource |
Description |
|---|---|
| African American Breast Cancer Alliance | A network creating culturally specific outreach to promote breast health awareness, patient support, and advocacy for African American breast cancer patients, survivors and their families. |
| American Indian Cancer Foundation | A collaborative organization that brings attention to Indigenous cancer burdens and solutions, advances capacity through training, technical assistance, and culturally-tailored resources, and increases availability of reliable Native-focused cancer data and solutions. |
| AMIGAS | A CDC bilingual educational outreach intervention designed to help community health workers increase cervical cancer screening among Hispanic and Latino/a/x people. |
| APPEAL | A national health justice organization working to advance equity in tobacco control and health for Asian Americans, Native Hawaiians, Pacific Islanders and other underserved communities. |
| Arab-American Family Support Center | A non-profit organization providing culturally and linguistically competent, trauma-informed, multigenerational social services to help Arab, Middle Eastern, North African, Muslim, and South Asian (AMENAMSA) immigrant and refugee communities find healthy paths to success and fulfillment. |
| Asian & Pacific Islander American Health Forum | A health advocacy organization influencing policy, mobilizing communities, and strengthening programs and organizations to improve the health of Asian Americans & Native Hawaiians/Pacific Islanders. |
| Asian American Cancer Support Network | A community network providing educational and supportive resources for Asian Americans affected by cancer. |
| Asian Health Coalition | A coalition of community-based organizations working to eliminate health disparities among AANHPI and other communities of color by supporting the development and implementation of culturally and linguistically appropriate health programs and initiatives. |
| Black Women’s Health Imperative | A program delivering evidence-based strategies, programs and advocacy to solve health issues that affect Black women and girls in the U.S. |
| CDC Health Literacy Communication Tactics | Recommendations from the CDC on ways to improve health literacy practices in patient messaging. |
| CDC Plain Language Materials & Resources | Resources and examples to help healthcare professionals implement plain language practices in patient communications. |
| Center for Black Health & Equity | A nationally recognized public health entity facilitating programs and services that promote health equity for Black and African American people, including tobacco cessation education and initiatives. |
| Gay and Lesbian Medical Association | A nationally recognized public health entity facilitating programs and services that promote health equity for Black and African American people, including tobacco cessation education and initiatives. |
| Health Equity Guiding Principles for Inclusive Communication | CDC guidelines to help public communicators ensure their messages adapt to the cultural, linguistic, environmental and historical situation of each population or audience of focus. |
| Latinas Contra Cancer | An organization working to eliminate health inequities by identifying and removing the obstacles Latino/a/x populations that are medically underserved face within healthcare systems. |
| Make it Your Own | A tool for helping medical professionals to create tailored health communications with evidence-based messaging and customized images. |
| National Cancer Institute | Providing resources for both patients and providers to help them understand prostate cancer, treatments, screenings, and statistics. |
| National LGBT Cancer Network | Improving the lives of LGBTQI+ cancer survivors through advocacy, education and training. |
| Nuestras Voces | An initiative of the CDC’s Networking2Save consortium of national networks implementing population-specific and public health-oriented strategies to impact the prevalence of commercial tobacco use and tobacco related cancers. |
| Nueva Vida | A nonprofit organization providing free, comprehensive, and culturally competent services to inform, support, and empower Latino/a/x families in the Washington, D.C. metropolitan area whose lives are affected by cancer. |
| PlainLanguage.gov | Government guidelines for using plain language with discussions of each subtopic. |
| Refugee Health Profiles | A comprehensive resource describing the demographic, cultural, and health characteristics of specific refugee populations. |
| SAGE for LGBTQI+ Elders | A national advocacy and services organization working to ensure a fulfilling future for the aging LGBTQI+ population. |
| Together, Equitable, Accessible, Meaningful (TEAM) Training | A training offered by the GW Cancer Center that aims to provide health care professionals with knowledge and strategies to support patient-provider communication and employ culturally competent practices. |
References
