Human Papillomavirus (HPV) & Prevention
Human papillomavirus, or HPV, is a common virus that is spread through intimate contact.1 Of the approximately 150 types of HPV currently identified, at least 40 occur in the genital area.2 HPV infections are extremely common, and most people will get HPV in their lifetime.2 Many HPV infections are asymptomatic and resolve on their own,2 but some persistent infections can cause cancers of the cervix, vagina, vulva, penis, anus, and throat.1 HPV is also responsible for a substantial portion of anogenital warts in the United States.2
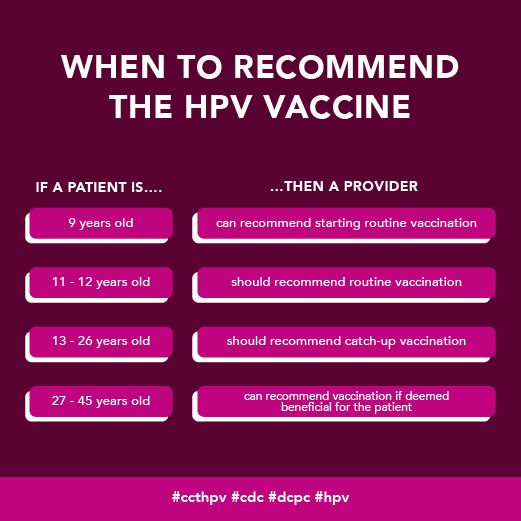
HPV vaccines can prevent both anogenital warts2 and 90% of cancers caused by HPV.3 Vaccination is recommended for all adolescents and young adults through age 26, with a first dose administered as early as age nine and a second dose administered six months later.3 Individuals who did not receive their first dose until after their 15th birthday should receive three doses given over six months.3 People ages 26-46 years old can discuss with their provider the risk of new HPV infections and if they would benefit from HPV vaccination.3
This health awareness social media toolkit can help your cancer control organizations implement evidence-based practices when communicating about HPV prevention.
Data and Statistics
More than 42 million people in the United States have a form of HPV that can cause other diseases, and 13 million Americans get HPV every year.1 HPV causes approximately 36,000 new cancer cases in the United States annually.1 Since the development of HPV vaccines, the rate of infections of HPV types that cause genital warts or cancer has dropped by 88% among teen girls and by 81% among young adult women.4 Among vaccinated women, incidences of cervical precancers caused by HPV types most commonly linked to cervical cancer have dropped by 40 percent.4 To date, more than 135 million doses of HPV vaccines have been administered in the United States.5
Best Practices for Communicating About HPV Prevention
- Provide a strong and understandable endorsement
-
- Recommend the HPV vaccine as you would any other vaccine. A provider recommendation is the single most important factor in whether parents choose to vaccinate their children.6 Studies show that a patient who receives a recommendation from a provider is four to five times more likely to receive the HPV vaccine.7
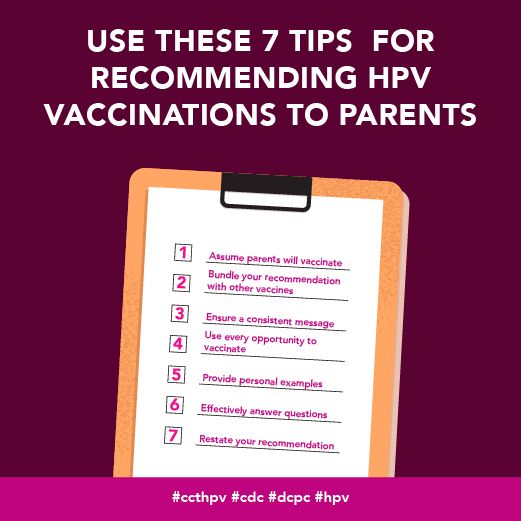
- Utilize a presumptive approach in which the provider assumes the parent wants to vaccinate instead of framing the recommendation as a question, as this tactic is shown to increase HPV vaccination acceptance among parents.8 Combining this approach with motivational interviewing and the sharing of informational resources can further increase vaccination rates.8
- Show a clear understanding of the vaccine and be able to explain its purpose in terms the parent will understand.9
- Be able to clearly explain current vaccine safety information.9
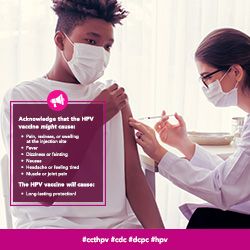
- Acknowledge minor risks and side effects.
- Ensure parents understand your recommendation is being made with the child’s best interest in mind.
- Frame non-vaccination as an active decision given the risk associated with not receiving the HPV vaccine.10
- Explain that the vaccine protects against cervical cancer, other cancers and genital warts (mentioning all three is more effective and compelling).9
- Have materials available for parents who have questions, including a list of credible websites parents or adolescents can use as a source of information. Visual aids can also help providers communicate complex information.9
- Emphasize the timeliness and urgency of vaccination
-
- Providers may vaccinate children against HPV as early as age nine.1 All children should be vaccinated by their 11th birthday or at the earliest age possible before age 26.
- Emphasize that vaccines are most effective when initiated before potential HPV exposure.
- Start conversations about the HPV vaccine by saying the child is due to receive their first dose, and if possible, bundle the recommendation with reminders about other vaccines.11
- Recommend that patients receive the vaccine during their visit, rather than suggesting a later date.11
- Explain the vaccine is most effective amongst teens and adolescents because they have the strongest immune response.9
- Continue to recommend the HPV vaccine, even if the parent has previously refused. Studies show that many parents eventually change their minds.12
- Recommend the vaccine for all patients, not just those perceived to be high risk.
-
- Recommend the vaccine for eligible patients regardless of sexual orientation or gender identity.
- Recommend the vaccine for eligible patients regardless of whether they are sexually active or not.
- Vaccine delay is more common among parents of cisgender girls than those of cisgender boys.12 Remind parents that their child is due for the vaccine during subsequent visits if the first dose was delayed.
Communicating with Diverse Audiences
Communication-related issues may also play a role in cancer disparities.13 Consider the information most useful to each diverse group (see below for specific messaging and read more on health disparities here). Tailor communication to these populations of focus with messages that also address conditions where these communities live, learn, work and play, as these social determinants of health can impact a wide range of health risks and outcomes. To ensure messages resonate with the coalition’s intended audience, we also recommend referring to the National Networks’ existing resources and adapting messages to reflect individuals with lived experiences.
- Black/African American Persons
-
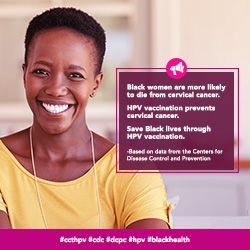
- Share information on the link between HPV and cervical cancer. Only 64% of Black patients reported knowledge that HPV can cause cervical cancer, compared to 81% of non-Hispanic White patients.14
- Encourage providers to discuss the HPV vaccine with Black patients. 75% of Black women indicated they were not recommended the HPV vaccine by a healthcare professional.14
- When sharing HPV and HPV vaccine information, prioritize government issued data and make sources clearly visible in your messaging. Black women are 7 times more likely to trust cancer information from government health agencies than white women and 9 times more likely to trust cancer information from religious organizations or leaders.14
- LGBTQI+ Persons
-
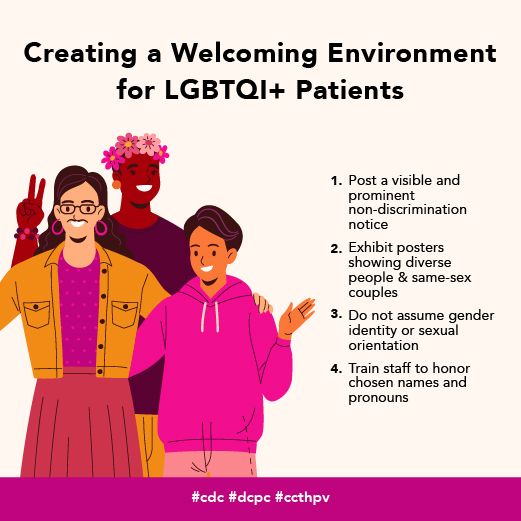
- LGBTQI+ patients and survivors report fears of social stigma as well as experiencing stigma within health care settings.15 Create messages that help health providers recognize and overcome implicit bias when communicating with patients about HPV vaccination. This may help to reduce stigma and to foster trust and honesty.
- Remind providers that gay and bisexual cisgender men should be offered the HPV vaccine. Studies show that 83% of men who have sex with men (MSM) received an HPV vaccine when recommended by a provider, compared to only 5% of MSM who did not receive a provider recommendation.16
- Encourage providers to recommend HPV vaccination among transgender patients. Transgender women (TGW) have significantly higher rates of HPV infection than cisgender men who have sex with men (MSM), with 98% of unvaccinated TGW showing evidence of current infection as compared to 81% of MSM.17 Among all transgender individuals, transgender men (TM) show the lowest vaccination rates with 20% of TM reported receiving at least one dose of an HPV vaccine, compared to 60% of TGW and 60% of non-binary/gender non-conforming patients.18
- Share information about self-sampling. New research on self-sampling for HPV shows promise in reaching rural women,19 and a recent review showed that self-sampling can be less distressing for #trangender men.20
- Hispanic/Latino/a/x Persons
-
- Inform providers about HPV vaccination disparities among Hispanic and Latino/a/x individuals aged 18 – 26 years to encourage more diligent recommendations for this group. Hispanic and Latino/a/x persons have the second-lowest rates of HPV vaccinations, with only 21.9% of patients having received at least one dose,21 despite over 40% of Hispanic and Latino/a/x individuals having a current genital HPV infection.22
- Provide Spanish-language resources and educational tools to Spanish-speaking parents of children eligible for HPV vaccines. Studies show that vaccine coverage is higher among Latino/a/x adolescents whose parents’ preferred language is Spanish, possibly due to increased adherence to provider recommendations among Hispanic and Latino/a/x individuals with less acculturation.22
- AANHPI (Asian American, Native Hawaiian/Pacific Islander) Persons
-
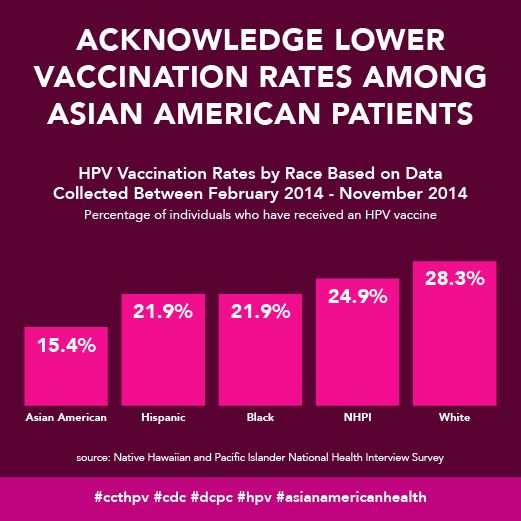
- Encourage providers to recommend HPV vaccines more proactively for AANHPI patients through age 26. Asian American individuals (disaggregated from NHPI individuals) are the most under-vaccinated demographic for HPV, with only 15.4% of patients having received at least one dose of an HPV vaccine, while only 24.9% of NHPIs have received at least one dose.21
- AANHPI girls aged 9-17 years were less likely to initiate HPV vaccination compared to White, Black, Hispanic and/or Latino/a/x girls.23
- AI/AN (American Indian, Alaska Native) Persons
-
- AI/AN youth aged 13-17 have comparatively higher rates of HPV immunization,24 compared to non-Hispanic White individuals in the same age range. However, rates of cervical cancer and cervical cancer mortality are higher for AI/AN patients.25 Recommend HPV vaccines as a form of cervical cancer prevention when communicating with this priority population.
- Age-based messaging
-
- Share the latest age-based recommendations for initiating HPV vaccinations to promote timely conversations with patients and parents.
- Gender-based messaging
-
- Remind providers to also recommend the HPV vaccine to individuals assigned male at birth, as well as their parents. Among cisgender male teens aged 13-17 years, about 60% were up to date with their HPV vaccination, compared to 64% for cisgender female teens aged 13-17 years.26 Only 10% of cisgender males aged 18-26 years received at least one dose of the HPV vaccine compared to 42% of cisgender females.21
HPV Messages and Graphics
Download All Messages and Graphics How to Post on Social Media
|
Topics |
Suggested Images |
|---|---|
|
Topic: Share the benefits of HPV vaccination #ccthpv #cdc #dcpc |

|
|
Topic: Provide age-based recommendations for HPV vaccination #ccthpv #cdc #dcpc |
|
|
Topic: Emphasize the importance of follow-up recommendations #ccthpv #cdc #dcpc |
|
|
Topic: Helping providers talk with parents about HPV vaccines #ccthpv #cdc #dcpc |

|
|
Topic: Provide HPV informational resources that providers can share with transgender men #ccthpv #cdc #dcpc #transhealth |

|
|
Topic: Tips for talking to parents about HPV vaccines #ccthpv #cdc #dcpc |
|
|
Topic: Resources for providers to share with parents #ccthpv #cdc #dcpc |
|
|
Topic: Provide parents with informational resources about potential side effects of the vaccine #ccthpv #cdc #dcpc |
|
|
Topic: Remind providers about the importance of HPV vaccinations for men #ccthpv #cdc #dcpc |
|
|
Topic: Reinforce the relationship between HPV and cervical cancer when recommending vaccinations to Black patients #ccthpv #cdc #dcpc #blackhealth |
|
|
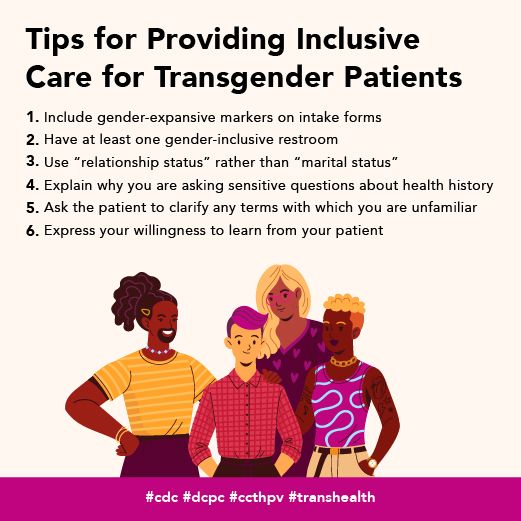
Topic: Tips for caring for LGBTQ+ patients #cdc #dcpc #ccthpv #lgbthealth |
|
|
Topic: Tips for caring for transgender patients #cdc #dcpc #ccthpv #transhealth |
|
|
Topic: Encourage cervical cancer screenings for transmasculine patients #ccthpv #cdc #dcpc |
|
|
Topic: Acknowledge lower vaccination rates among AANHPI patients #ccthpv #cdc #dcpc #asianamericanhealth |
|
|
Topic: Provide Spanish-language resources to increase HPV vaccination coverage among Hispanic/Latino/a/x patients #ccthpv #cdc #dcpc |

|
|
Topic: Recommend HPV vaccination as a form of cervical cancer prevention among AI/AN patients #ccthpv #cdc #dcpc #aianhealth |

|
|
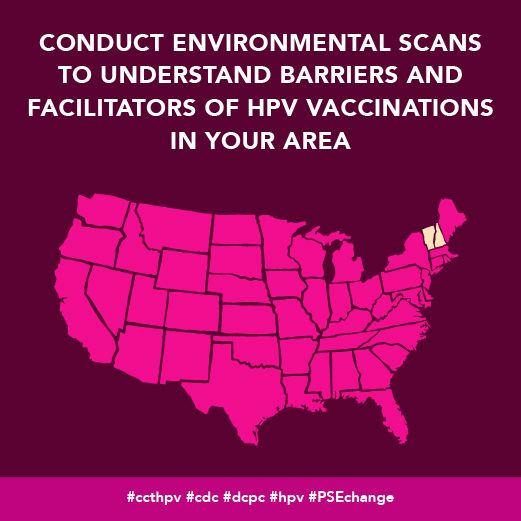
Topic: Policy, Systems and Environmental (PSE) Change #ccthpv #cdc #dcpc #PSEchange |

|
|
Topic: Policy, Systems and Environmental (PSE) Change #ccthpv #cdc #dcpc #PSEchange |
|
| Topic: Using recall/reminder activities to boost vaccination rates Reminder and recall systems are effective for both your costs and your patients! Research shows that activities like personal phone calls, text messages, postcards, and more can boost #vaccination rates. Try using these recall/reminder resources from the American Academy of Pediatrics to encourage HPV vaccinations in your area. https://tinyurl.com/ftj56fpy |
|
Download All Messages and Graphics How to Post on Social Media
How to Post to Social Media
Start by downloading the ZIP file above. Then double click the downloaded file to unzip and open the folder. Inside, you’ll find three CSV files.
- Messaging.csv contains captions for all messages in the toolkit, organized by topic.
- Bulk - Instagram.csv contains captions for all Instagram messages, along with graphics URLs that can be used to bulk schedule both text and images.
- Bulk - LinkedIn-Facebook.csv contains captions for all LinkedIn, Facebook, and Twitter messages, along with graphics URLs that can be used to bulk schedule both text and images.
- Bulk - Twitter.csv contains captions for all Twitter messages, along with graphics URLs that can be used to bulk schedule both text and images.
Inside the main folder, you’ll also see two sub-folders containing the messaging graphics for all major platforms. The first folder contains rectangular images suited for use on Facebook, Twitter, and LinkedIn. The second folder contains square images suited for Instagram.
Select your platform below for additional instructions.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Facebook. If you aren’t already logged in, enter your email address (or phone number) and password, then tap “Log in.”
- Tap the post box. This box is at the top of the News Feed. If you're posting to a group, you’ll find the box just below the cover photo. There will generally be a phrase like “Write something”or “What’s on your mind?” in the box.
- Tap “Photo/Video” near the middle of the post screen, then select the downloaded graphic to upload and tap “Done.” Doing so adds the photo to your post.
- Tap “Post.” It’s in the top-right corner of the screen from the app, or the bottom-right from your computer. Doing so will create your post and add it to the page you’re on.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Twitter. If you aren’t already logged in, enter your email address and password, then tap “Log in.”
- Tap the post button. This button is at the bottom right of the News Feed. There will generally be a phrase like “What’s happening?” in the box.
- Tap the camera icon near the middle of the post screen, or the picture icon in the bottom left of the post screen then select the downloaded graphic to upload, and add the post caption.
- Tap “Tweet.” It’s in the top-right corner of the screen from the app, or the bottom-right from your computer. Doing so will create your post and add it to the page you’re on.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open Instagram. If you aren’t already logged in, enter your username (or phone number) and password, then tap “Log in.”
- Tap the plus sign box. This box is at the top right. Select the downloaded graphic or drag it into the box to upload it.
- Select “Square (1:1)” for the aspect ratio, then click “Next.”
- Ignore the filters screen, then click “Next” again.
- Paste the caption where it says, “Write a caption…” at the top.
- Under “Accessibility,” consider adding alt text to describe the photo for people with visual impairments.
- Tap “Share.” It's in the bottom-right corner of the screen.
-
- Download the suggested graphic.
- Highlight the corresponding message with your cursor. Right click and select “Copy.”
- Open LinkedIn. If you aren’t already logged in, enter your email address and password, then tap “Log in.”
- Tap “Start a post” from the main share box. This box is at the top of your profile.
- Tap “Photo” from the top of the post screen, then select the downloaded graphic to upload and tap “Done.” Doing so adds the photo to your post.
- Tap “Post.” It's in the the bottom-right. Doing so will create your post and add it to the page you’re on.
- Bulk Scheduling
-
Social media management tools like Hootsuite and Sprout Social offer bulk scheduling options for uploading multiple messages at once. The spreadsheets included in the download can be adapted to fit multiple scheduling platforms or services. They are currently formatted to work with Sprout Social’s bulk scheduling option. Please review the bulk scheduling format requirements for your specific platform before posting. Messages are sorted by network.
HPV Resources
|
Resource |
Description |
|---|---|
| Equality California's Diversity, Equity, and Inclusion Program | A free, online LGBTQ+ HPV training, “Increasing Vaccination Rates for the LGBTQ+ Community.” This curriculum outlines evidence-based, LGBTQ+ sensitive strategies for increasing HPV vaccination rates among adolescents. Training engages and trains healthcare workers in evidence-based, LGBTQ+ sensitive practices to encourage HPV vaccination, and to increase HPV vaccination rates among LGBTQ+ populations, particularly transgender and gender-nonconforming youth. |
| Gay and Lesbian Medical Association | A group dedicated to ensuring health equity for LGBTQ+ people through research, advocacy, and education. GLMA also shares resources for both patients and providers caring for LGBTQ+ people. |
| HPV Cancers Alliance | Sharing education and resources to increase HPV vaccination rates and prevent HPV-related cancers. |
| HPV Information for Parents | CDC education on HPV, vaccines, and HPV risks to encourage parents to give their children the HPV vaccine. |
| HPV Resources for Professionals | CDC tools and guides healthcare professionals can use to communicate accurate information with their staff members and the parents of adolescent and young adult patients. |
| “HPV Vaccination” Cancer Plan Tip Sheet | Tip sheet used to help CCC program staff, coalition staff, and volunteers update their CCC plans. The Tip Sheet includes tips about engaging partners, identifying and using the right data, setting baselines and targets, and crafting objectives and strategies, as well as a list of practical questions to guide discussion on the topic with your coalition. |
| Immunize.org Vaccine Information Statements | Providing CDC curated HPV Vaccine Information Statements in English and 33 other languages. |
| Make it Your Own | A tool for helping medical professionals to create tailored health communications with evidence-based messaging and customized images. |
| The National Cervical Cancer Coalition | Helping women, family members and caregivers battle the personal issues related to cervical cancer and HPV and advocating for cervical health in all women. |
| National LGBT Cancer Network | Improving the lives of LGBTQ+ cancer survivors through advocacy, education, and training. |
| NOMAN Campaign | A campaign aiming to increase HPV vaccination rates for all genders, promote parent education, and influence policy related to HPV vaccinations. |
| Pap-a-thon Toolkit | Hosting a Women’s Community Health Event – Increasing Cervical Cancer Screening in Rural Tribal Communities (itcmi.org) |
| Path to a Bright Future: HPV Cancer Prevention | Addresses opportunities for HPV prevention, HPV vaccination and increasing vaccination coverage, and the St. Jude HPV cancer prevention program (use passcode C2NTM*&v to access) |
| Queer Health is Power Social Media National Partner Packet | A new set of social media shareables focused on access to care, LGBTQ+ screening, and HPV. This project was piloted in New York and is now available for national use. |
References
